Background: Pediatric orbital cellulitis/abscess (OC) is a known complication of sinusitis that can have detrimental outcomes such as vision loss and intracranial extension if not diagnosed and treated promptly. In many patients with OC, the microbiologic data is not available to guide provider selection of targeted antibiotics, so variation in prescribing patterns exists. Many institutions use combination parenteral (IV) antimicrobial therapy that includes coverage against methicillin-resistant Staph aureus (MRSA). A recent study using a large inpatient database showed that the most frequently prescribed regimens for OC are vancomycin alone or in combination (43.1%) and a clindamycin/beta-lactam combination (30.9%). Only 10% of the participating hospitals did not use MRSA active antibiotics. The purpose of our study was to identify the prevalence of MRSA in pediatric OC in order to guide improved selection of empiric antibiotics.
Methods: a. A retrospective case series was conducted at a large academic center in the Midwest. Patients age 2 months to 17 years admitted with a CT-confirmed diagnosis of OC between January 2013 and December of 2019 were included in the study. Patients with eye trauma, prior eye surgery, eye prosthetics, or immunocompromise were excluded. Microorganisms from intra-operative cultures (orbit and/or sinus) were analyzed and the local prevalence of MRSA was calculated. b. The prevalence of MRSA OC in other US states was calculated using previously published studies. Studies were identified through a systematic literature review that followed the PRISMA guidelines. The search strategy included MeSH terms and keywords related to orbital or subperiosteal cellulitis/abscess and children. To be included, studies had to report pediatric OC data exclusively or separate from adult data. Cultures reported had to be from intra-operative orbital or sinus specimens. Studies reporting only nasal, conjunctival, or other surface cultures were excluded. Studies published before year 2000 and those with study period before 1990 were excluded.
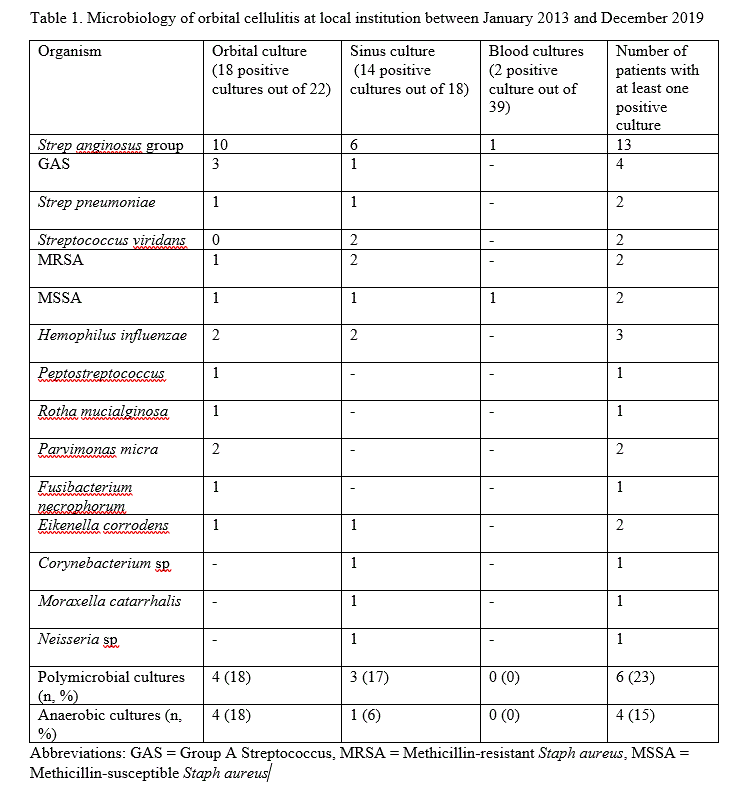
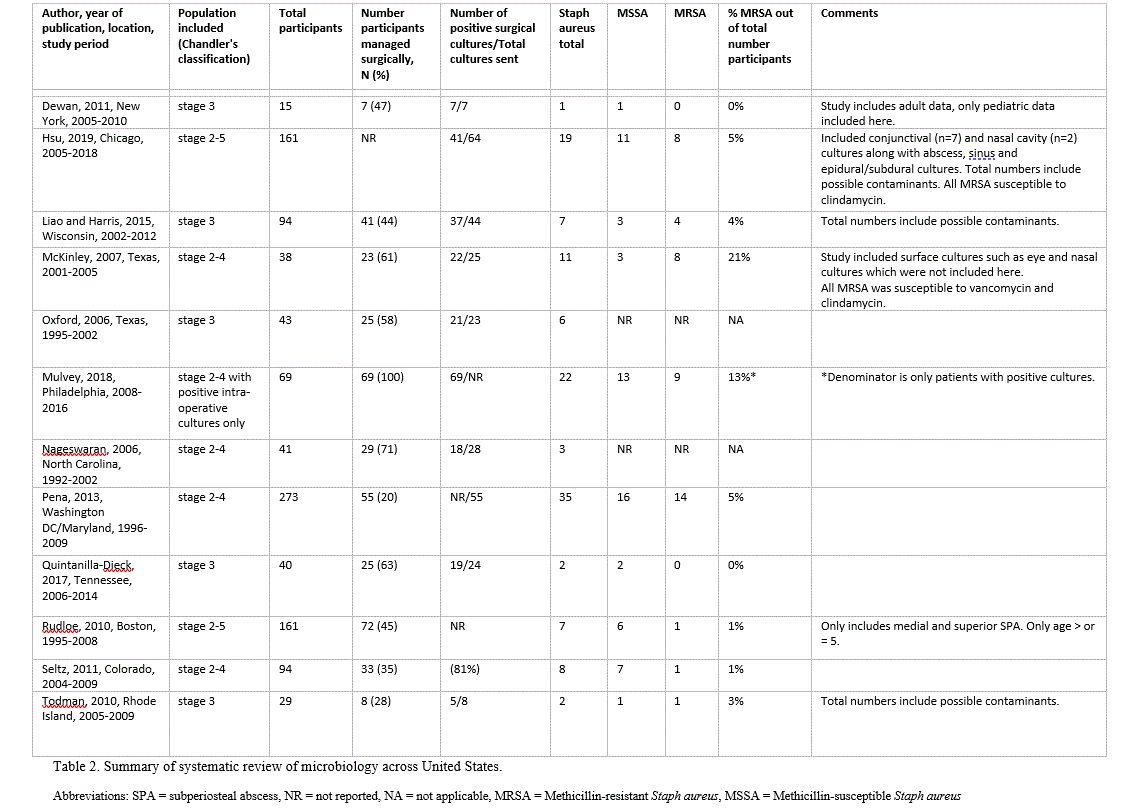
Results: a. Ninety-five patients with OC were included in the case series. Median age was 8.1 years (IQR 4.6-11.4). Sixty-seven percent of patients were males and 65% had a subperiosteal abscess (SPA). Forty-two percent of patients with SPA required surgical management. The most common organism recovered from surgical culture was Strep anginusus, followed by Staph aureus and Group A Strep (Table 1). Local MRSA OC prevalence was 2% (2 out of 95 total patients), similar to 3% at the same institution in 2002-2012. Eight percent of surgical cultures grew MRSA (2 out of 26), similar to 10% for 2002-2012. b. Twelve articles representing 11 US states were included in the systematic review; nine were case series and three were retrospective cohort. MRSA prevalence varied from 0% in a study based in New York state to 21% in a study based in Texas (Table 2). Note that when the study population includes SPA only, the prevalence calculated is an overestimate of total MRSA OC prevalence.
Conclusions: With the low prevalence of MRSA OC in some regions of the country, patients with mild disease and without risk factors for MRSA infection may not require dual therapy that includes MRSA coverage.