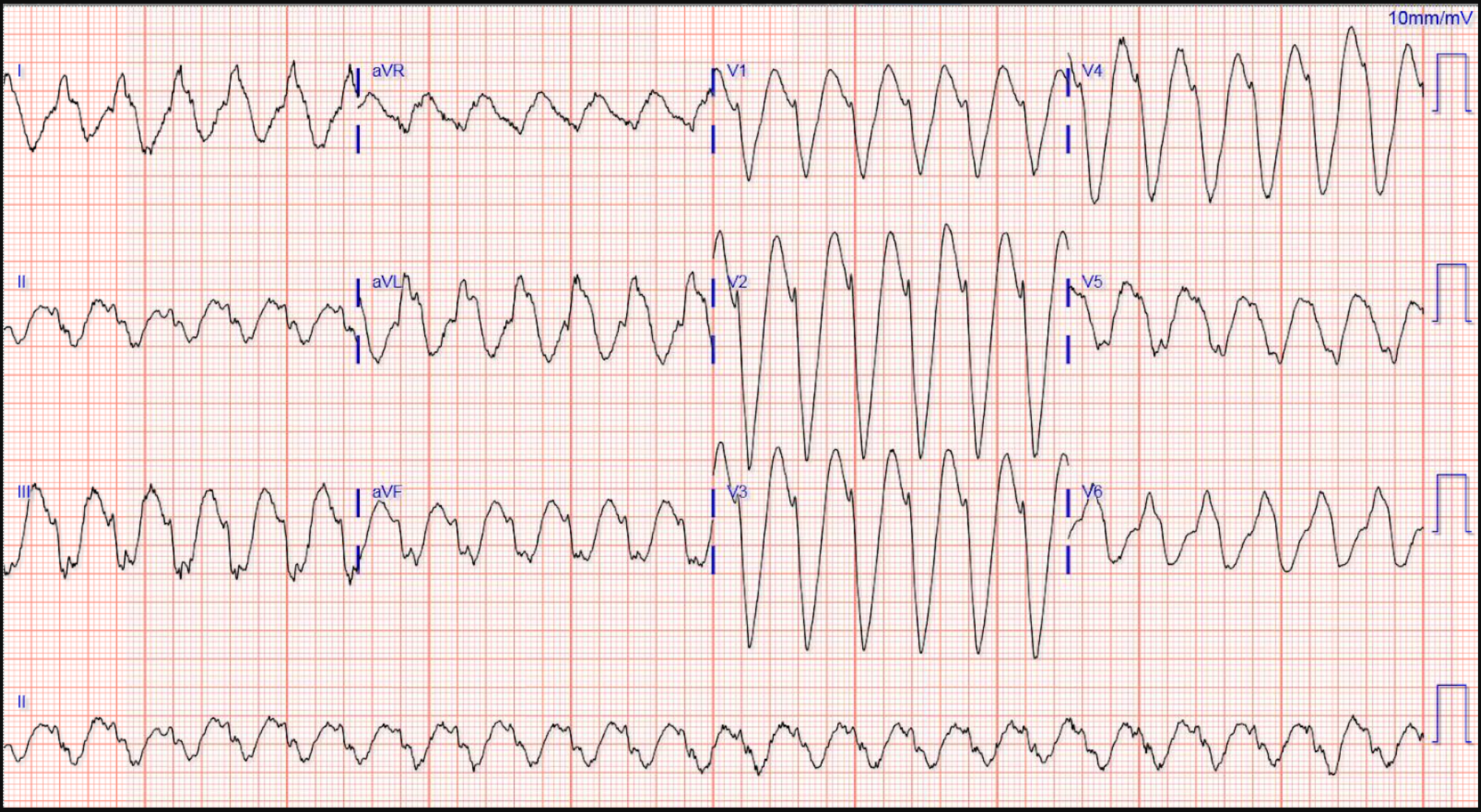
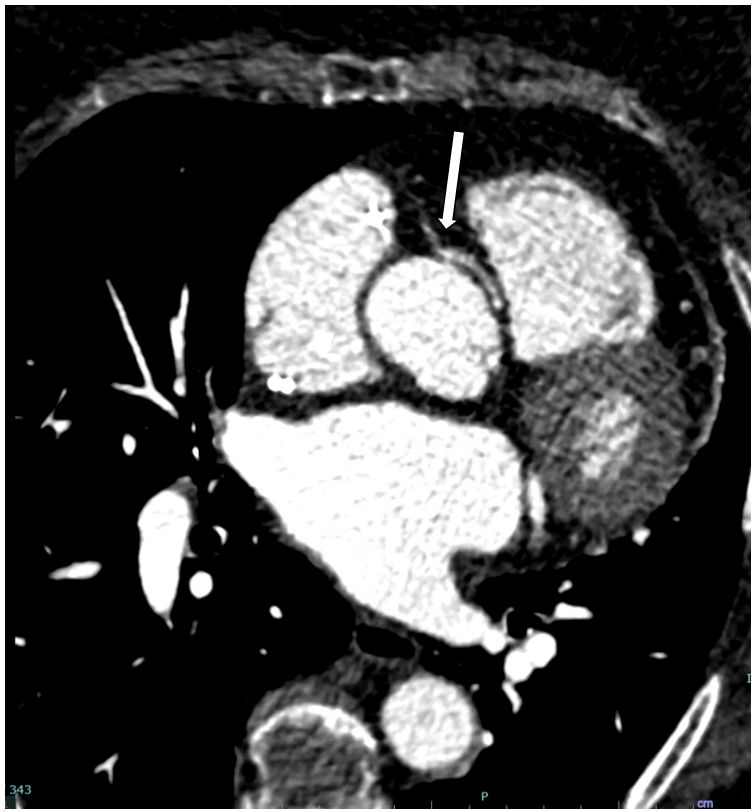
Case Presentation: A 77-year-old female with atrial fibrillation (AF) on flecainide, sinus node dysfunction (SND), and permanent pacemaker presents with frequent palpitations. EKG showed regular, wide-complex tachycardia with ventricular rate of 137 BPM. Device interrogation revealed atrial flutter with 1:1 AV conduction (AL11AV). Rhythm terminated with overdrive atrial pacing along with resolution of symptoms. Troponins noted to be mildly elevated prompting ischemic evaluation. Stress perfusion imaging revealed transient ischemic LV dilation. Catheterization and CT Coronary revealed AAORCA without coronary artery disease (Figure 2). Flecainide changed to amiodarone with improvement in symptoms.
Discussion: Anomalous, intraarterial origin of the right coronary artery (AAORCA) is a rare condition with an estimated prevalence of 0.28%. Patients with ARCA are at increased risk of sudden cardiac death (SCD) from fatal arrhythmia most often induced during strenuous exertion. This is due to transient ischemia from mechanical compression of the anomalous vessel as it courses between the PA and aorta which increase in diameter during systole. This can manifest as transient ischemic dilation (TID) on stress MPI despite disease-free coronary arteries on angiography. Patients with diminutive anomalous vessels may be even more at risk for stress-induced ischemia given diminished flow reserve at baseline. CT coronary or Cardiac MRI imaging can be used to further detail coronary anatomy (specifically vessel course and luminal caliber/patency) if abnormal anatomy is suspected on angiography. SND can develop overtime due to chronic ischemia of the SA node supplied by AAORCA predisposing to the development of AF. The use of flecainide for AF rhythm-control is contraindicated in the setting of structural and ischemic heart disease due to its rate-related, pro-arrhythmogenic effects in ischemic myocardium, ability to promote AL11AV by slowing AF rate and AV conduction (worsening ischemia from rapid ventricular rates), and increasing pacing thresholds leading to cardioversion and overdrive pacing resistant ventricular arrythmias. Given these effects, flecainide should be avoided in patients with AAORCA as it can predispose to potentially life-threatening tachyarrhythmias. Amiodarone may be a reasonable alternative as it does not share the same pro-arrhythmic effects.
Conclusions: Flecainide can lead to significant arrhythmia in patients with AAORCA and further workup should be considered in patients with undefined coronary anatomy