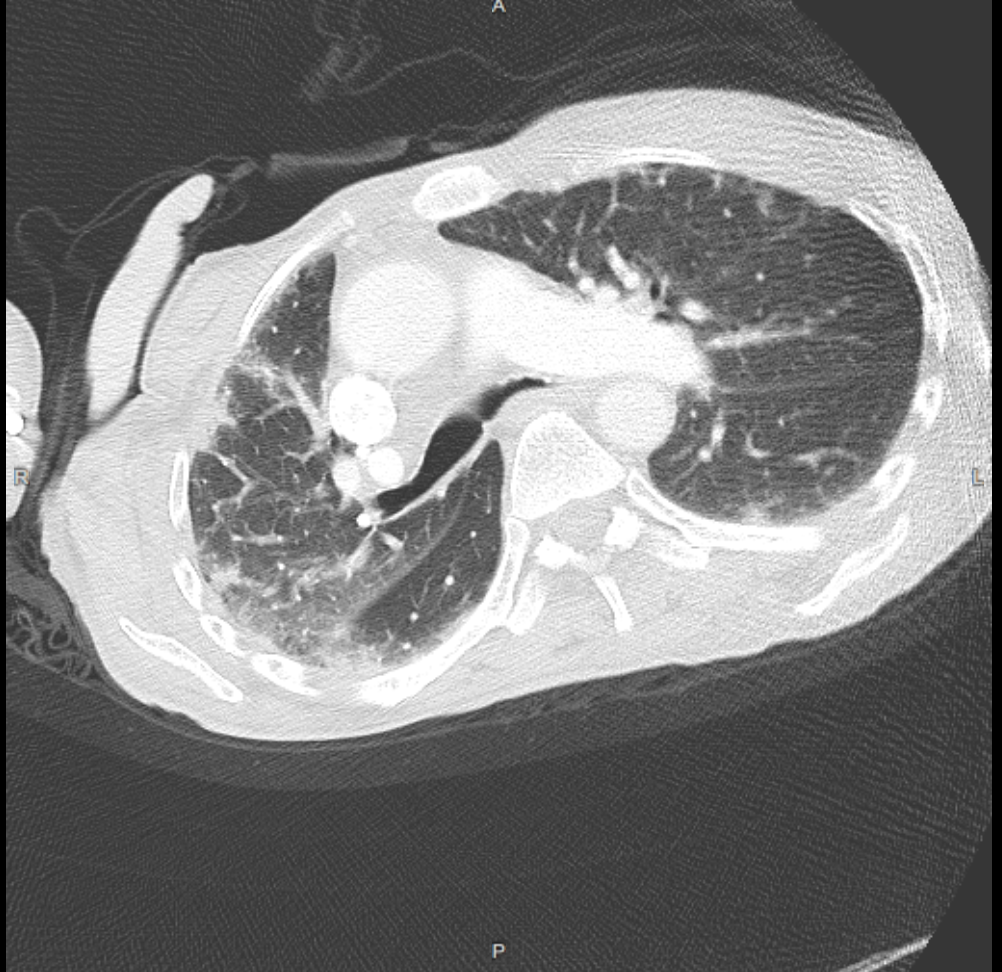
Case Presentation: 64-year-old female with a past medical history of cerebral palsy presented with recurrent fever. One week earlier, she had been hospitalized for sialadenitis and pneumonia and completed a 10 day course of antibiotics. Family reported recurrent fevers (Tm 102F) after discharge with associated mucosal ulcerations and chronic intermittent joint pain. She did not have any associated cough, shortness of breath, or chest pain. On exam, she was very thin, minimally verbal, and bed bound with significant diffuse muscle atrophy. She was tachycardiac with bilateral pulmonary rhonci and non-pitting left lower extremity swelling that was non-erythematous and non-tender. Livedo reticularis of her lower extremities was noted bilaterally. There was no lymphadenopathy or palpable salivary glands. ESR and CRP were elevated at 65 and 14 respectively. Her WBC was normal at 5.1. CMP and TFTs were normal. Creatine kinase was normal at 125, aldolase was normal at 4.8. Respiratory viral panel with COVID-19 was negative. Urinalysis was negative for pyuria or hematuria. CT neck showed persistent enlargement of the right submandibular gland. CT Chest showed patchy bilateral peripheral based reticular and airspace opacities, increased from prior and consistent with pneumonia. A PE was not seen. Given her persistent fevers and CT findings, she was started on empric broad spectrum antibiotics for pneumonia vs recurrent sialadenitis. However, fevers persisted despite antibiotic therapy. Pulmonology was consulted, and felt her CT lung findings likely represented a non-infectious Nonspecific Interstial Pneumonia (NSIP). Rheumatology assisted in evaluating autoimmune etiologies. ANA, anti-CCP, dsDNA, Smith, RNP, SSA/SSB, Scl70, Jo1, anti-centromere, and ANCA antibodies were all negative. A myositis panel was positive for the MDA5 antibody. MRI of the bilateral femurs showed bilateral muscular edema with enhancement consistent with myositis. Muscle biopsy was deferred. She was diagnosed with MDA5 dermatomyositis. Antibiotics were discontinued, and she was started on prednisone with outpatient plans to initiate Tofacitinib. Although CPK and aldolase were within the normal reference range, it was felt that they may have been relatively elevated in our patient given her muscle atrophy.
Discussion: Dermatomyositis is an autoimmune disorder characterized by proximal muscle weakness, myopathy, and rash. MDA5 dermatomyositis is a sub-type that often presents with absence of myopathy but has a strong association with ILD with a NSIP pattern on imaging, which was present in our patient. Along with ILD, patients with anti-MDA5 antibodies also have an increased risk of oral pain and/or ulceration, hand swelling, arthritis/arthralgia, and diffuse hair loss. Treatment, as with most autoimmune disorders, involves immunosuppression.
Conclusions: Our patient was a diagnostic challenge. She was initially diagnosed with pneumonia. However, failure on broad antibiotic therapy led us to reassess our diagnosis. Furthermore, it was critical to retain myositis within the differential despite a normal CK level given our patient’s significant muscle atrophy. She was ultimately diagnosed dermatomyositis with a normal CK level, which is an uncommon presentation of an uncommon disease. Our case highlights the importance of both maintaining a broad differential and reassessing your diagnosis when the clinical course does not proceed as expected. These skills our critical in the field of Hospital Medicine.