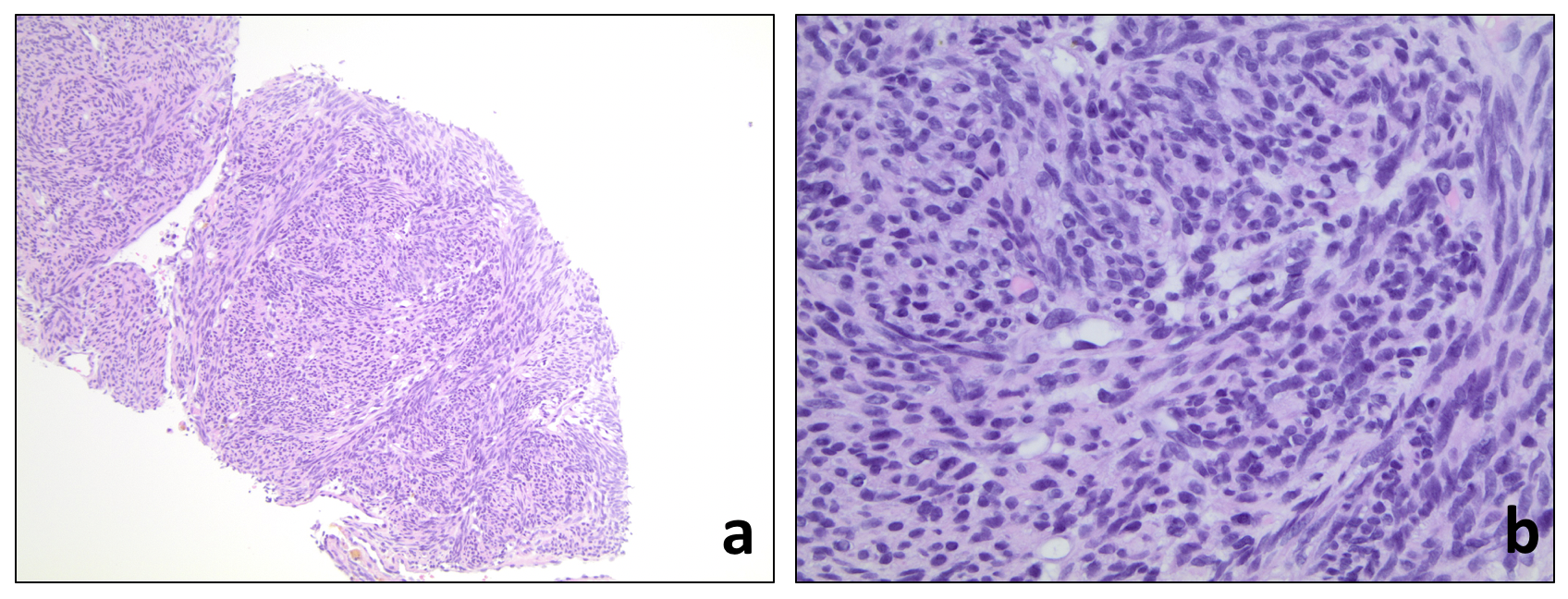
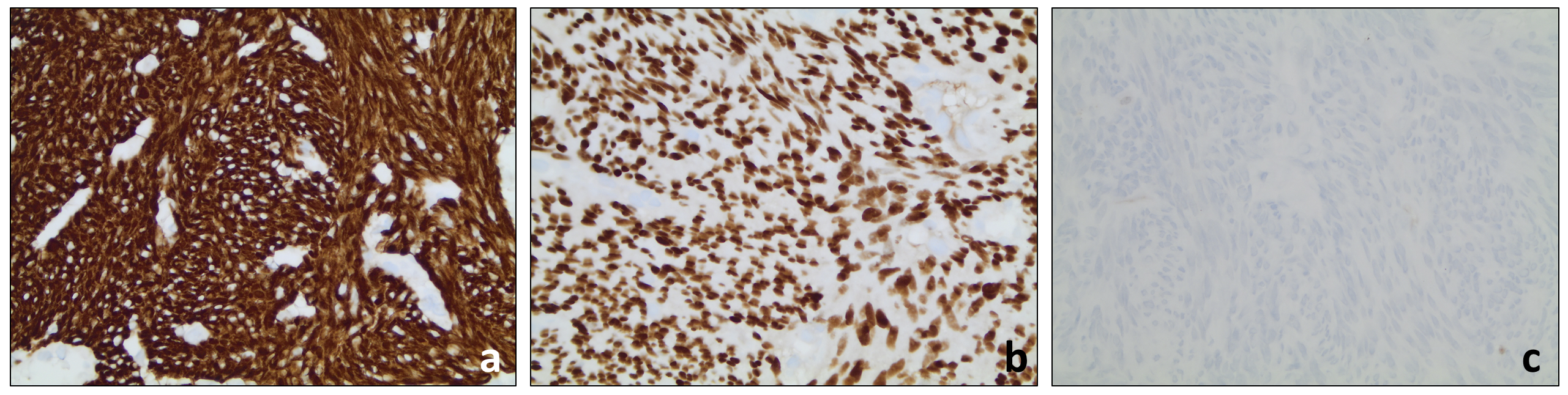
Case Presentation: A 73-year-old woman with past medical history of hypertension, deep venous thrombosis and chronic kidney disease presented with nausea, vomiting, abdominal distension, weight loss and progressive deconditioning. Physical exam showed temporal wasting, abdominal distension with fluid wave, upper extremity sarcopenia, 3+ bilateral lower extremity edema, and generalized weakness impairing ability to walk. Creatinine was 3.43, Hgb 8.5, LFTs were within normal limits, and iron studies were inconsistent with iron deficiency. CA-125 was elevated (286); however, CEA, CA19-9, AFP were within normal limits. Renal ultrasound showed no evidence of hydronephrosis or renal calculi. CT abdomen and pelvis without contrast showed a large left pelvic mass and massive ascites. MRI imaging of the pelvis in this case was suggestive that the mass was of uterine origin. Paracentesis was performed and ascitic fluid cytology showed no malignant cells. CT guided core biopsy of the pelvic mass showed a smooth muscle tumor consistent with a uterine leiomyoma [Fig. 1, 2]. Gynecology consultation relayed that the patient was not a surgical candidate due to poor performance status. The patient went on to have pleural effusions and new-onset seizures refractory to levetiracetam. MRI imaging of the brain showed a left cerebellar infarct, and a serum autoimmune encephalitis panel was negative. Unfortunately, our patient then developed worsening renal failure and progressive encephalopathy leading up to her death 2 weeks later.
Discussion: Ascites and weight loss are common presenting symptoms that prompt hospitalization and inpatient work-up. Congestive heart failure, liver failure, renal failure and malignancy are usually at the top of a hospitalist’s differential diagnoses for these symptoms. However, this case demonstrates a rare etiology of ascites that must be considered in female patients. Our patient’s ascites was due to Pseudo-Meigs syndrome, defined by the triad of a benign or malignant non-ovarian tumor, ascites, and pleural effusion. Since originally defined [ref.1] by Dr. Meigs himself in 1954, less than 25 cases of Pseudo-Meigs syndrome due to uterine leiomyoma have been reported [ref.2]. Review of these cases in the literature show that in the majority of reported cases, the syndrome was diagnosed with sufficient time to offer definitive surgical intervention. In these cases, surgical resection was curative of Pseudo-Meigs syndrome with subsequent decrease in CA-125 levels [ref.3]. In cases of unrecognized and untreated Pseudo-Meigs, patients may be subject to multiple paracenteses or thoracenteses, resulting in complications such as infection, bleeding, and hypoalbuminemia. Furthermore, continued growth of the tumor, whether benign or malignant, may cause additional complications.
Conclusions: This case highlights a very unusual etiology for ascites as well as an unusual end stage manifestation for uterine fibroids, mimicking what is usually observed in patients with underlying malignant conditions. Unfortunately, by the time our patient presented and her diagnosis of Pseudo-Meigs syndrome was recognized, her condition had deteriorated to the point that she was not eligible for curative surgical resection. This circumstance highlights the importance of early identification and treatment of this condition so that curative resection can be pursued.