Background: Since the publication of the Institute of Medicine report To Err Is Human in 1999, preventable inpatient deaths in the United States have been estimated as between 44,000 and 98,000 deaths annually. A more recent review concluded that the number of preventable deaths was over 250,000 cases annually. Critics have pointed out that these estimates are based on studies with methodologic limitations. Nevertheless, because inpatient deaths are believed to be commonly due to medical error, and therefore preventable, adjusted mortality rates are used for hospital rankings by both the Centers for Medicare and Medicaid services (CMS) and the Veterans Administration (VA). Given the uncertainty in reported rates of preventable inpatient mortality, we undertook a systematic review and meta-analysis of studies that directly assess rates of preventable mortality in hospitalized patients.
Methods: A systematic literature search was conducted for studies that reported case series of hospitalized patients who died and used physician review to determine the number of patients who died due to preventable medical errors. Our search included MEDLINE, EMBASE, Web of Science, and the Cochrane library from database inception through July 3, 2018. Study quality was assessed using the Newcastle-Ottawa Quality Assessment Scale. The mortality rates were pooled using random-effects meta-analysis and heterogeneity was estimated using the I² statistic.
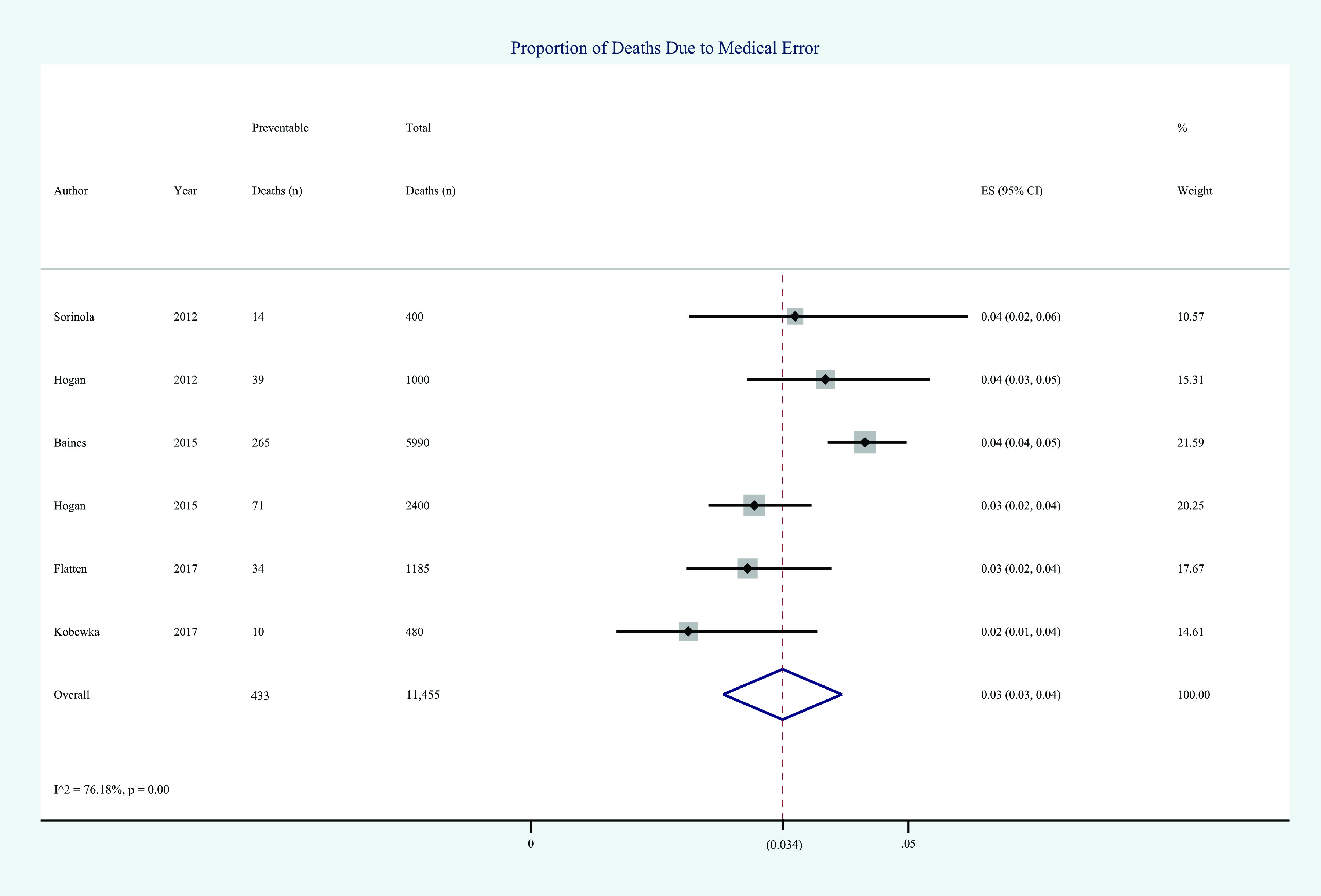
Results: 1,086 studies were screened for inclusion. Six studies including 11,455 patient deaths met study inclusion criteria. The overall pooled rate of mortality due to preventable error was 3.4% (95% CI 2.7% – 4.2%) (figure 1). Two studies reported rates of preventable mortality limited to patients expected to live longer than three months. The rate of preventable mortality for these patients was 0.8% (95% CI 0.3% – 1.9%). In the United States, these estimates equate to approximately 21,450 preventable deaths annually and 5,720 deaths among patients with greater than three-month life expectancy.
Conclusions: Based on our review, the number of deaths due to medical error is much lower than previously reported. Furthermore, most of these preventable deaths appear to occur in patients with less than three months life expectancy. Because the vast majority of inpatient deaths are not due to medical error, overall hospital mortality rates are unlikely to be valid quality measures. Variation in mortality rates are more likely to reflect differences in patient characteristics and factors that determine the location of patient death such as availability of hospice. Our results also question the validity of using disease specific mortality rates for quality measures and reimbursement, as currently done by CMS.