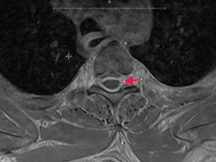
Case Presentation: 48-year-old man with past medical history of AIDS, unknown recent CD4 count presented to the ED complaining of slurred speech and disorientation for 3 days associated with fever and generalized body ache. Patient was admitted for stroke workup (CTH, CTA head/neck, and MRI brain) which resulted negative and there were also concerns for pneumonia. Patent was started on antimicrobials. Pulmonology and Infectious Disease were following. The patient was noted to have generalized weakness, but he could sit to stand with moderate assistance. On day 3, patient started complaining of severe headache and neck stiffness. Lumbar puncture was ordered to evaluate for meningitis which showed yellow color CSF with xanthochromia, protein 1862, glucose 18. Due to xanthochromia of CSF and a concern for Subarachnoid hemorrhage, CT Head was ordered. Meanwhile, the patient developed new onset weakness of bilateral lower limbs and slurring of speech. So, he also underwent a repeat CT head, CTA and MRI brain, and CT Lumbar Spine, which were all negative. Patient was transferred to ICU for closer monitoring. Meanwhile, patient’s CD4 count resulted to be 10. CSF studies showed VDRL reactive with IgG positive West Nile virus. Neurology was consulted. On day 5, the patient was much more stable and was transferred out of ICU. Patient continued to complaint of neck pain and reported back pain. His bilateral lower limbs were still weak with decreased sensation, and he had new onset bowel bladder incontinence. Keeping in mind, the differential of Froin’s syndrome and his persistent lower extremity weakness, MRI multi-level spine was ordered which showed a 14.5cm multiloculated peripherally enhancing extradural lesion extending from C7 to T6 resulting in critical spinal canal stenosis highly suggestive of an epidural abscess. The patient was emergently transferred to neurosurgical center and had the C7 left hemilaminectomy with T1-T6 laminectomy done on the same day of transfer. Patient made gradual improvement and was later discharged to a rehab after 13 days of hospital stay.
Discussion: Xanthochromia along with elevated proteins, hypercoagulable CSF on lumbar puncture is the triad of Froin’s syndrome. These classical findings can lead towards the diagnosis of meningitis, spinal tumors, spinal epidural abscess, trauma, Guillain Barre syndrome, multiple myeloma. [1,2,] Described in 1910 by Georges Froin, this syndrome is often overlooked. [3] The Froin’s Syndrome triad on our patient alerted us to perform further workup and helped us diagnose a neurosurgical emergency.
Conclusions: The pathophysiology behind Froin’s syndrome is thought to be due to meningeal irritation and stagnant CSF causing passive and/or active diffusive processes, resulting in hyperproteinosis and hypercoagulation. Protein levels greater than 500 mg/dL usually indicate defective CSF recirculation and spinal block. This can indicate a spinal obstruction in the forms of abscesses, tumors, degenerative stenosis, or herniations. [2,4] Froin’s Syndrome is a rare entity with only 17 case reports reported and published, on our search. When identified in a patient, clinicians should be vigilant towards probable spinal lesions, which could be obstructive, even a spinal emergency. In our patient, the combination of clinical exam findings and CSF suggestive of Froin’s syndrome, guided us to order a multilevel spine MRI, which identified the large, impinging epidural abscess.