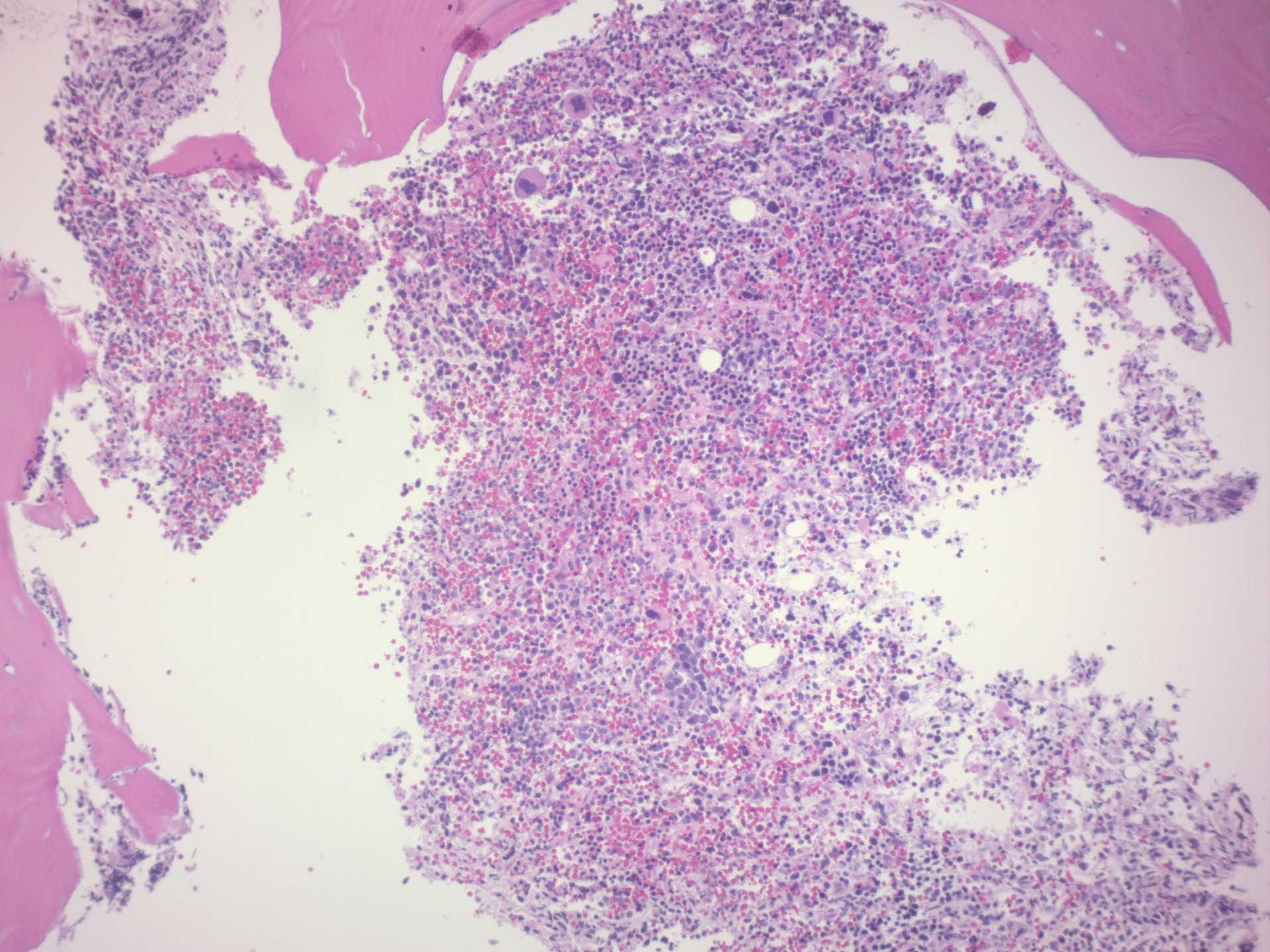
Case Presentation: A 66-year-old male with a past medical history of hypertension, atrial fibrillation, and diabetes initially presented to the hospital with shortness of breath, fatigue, and several episodes of bloody stool after two weeks of intermittent bloody stool at home. He reported that he had seen his PCP who had initiated a workup but as the patient had more heavy and frequent bloody bowel movements, he presented to the hospital. He denied any history of EGD or colonoscopy. Initial lab work showed that he had normocytic anemia with a hemoglobin of 8.5 and severe thrombocytopenia with a platelet count of 10. On manual differential, there was markedly decreased platelets with normal platelet morphology but findings were otherwise normal. Patient was admitted to the hospital and underwent CTA abdomen which showed the patient had no acute GI bleed but incidental finding lucency within the right posterior iliac bone measuring approximately 1.9 cm which was non-specific. Initially, it was suspected that the patient had ITP and he underwent platelet transfusion with steroids without improvement. Patient was then tried on IVIG therapy but continued to have unstable platelet levels and bloody bowel movements. Unfortunately, due to his low platelet count, the patient could not undergo a colonoscopy. During his hospital stay, the patient developed altered mental status and was upgraded to the ICU for higher acuity care and sedation. As the patient was not responding to therapy, further workup was initiated. Flow cytometry was performed which showed mildly increased myeloid cells. Bone marrow biopsy was pursued which initially resulted in a dry tap before the second attempt did show abnormal fragmented hypercellular marrow tissue with increased mononuclear cells positive for CD20, CD34, PAX5, and TdT (weak) and mild reticulin fibrosis – all suggestive of AML. After a discussion with hematology and family, the patient was transferred to a specialized facility for inpatient chemotherapy.
Discussion: Although not a common diagnosis, AML, once symptomatic, is a relatively recognizable disease identified by both clinical and laboratory findings. However, in this incident, the patient had an unusual presentation in both. Clinically, the patient’s first initial symptom was rectal bleeding. Literature review does recognize bleeding as one of the initial symptoms, however typically it is more associated with gum or nose bleeding, and only advanced cases of AML have heavy internal bleeding. Additionally, on lab work, patients with AML typically have blasts seen on blood smear, which was not found in the patient, which is why the initial diagnosis was thought to be ITP.
Conclusions: This case demonstrates an atypical presentation of a deadly disease process that is vital to identify quickly for lifesaving treatment.