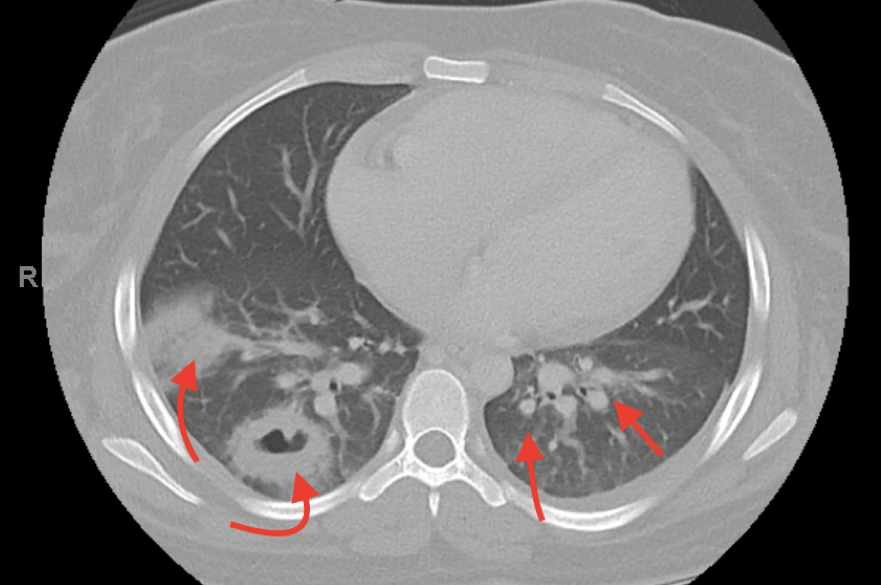
Case Presentation: 18-year-old female presented with one week of fever, left flank pain, and sore throat. On arrival she was febrile, tachycardic, hypotensive, and tachypneic. Physical exam was notable for left flank tenderness, labial and buccal ulcerations. Labs were significant for positive urinalysis, leukocytosis, blood cultures with gram negative bacteria, and recent negative streptococcus rapid test. The patient was started on Vancomycin, Cefepime, and Metronidazole due to concern for sepsis in the setting of pyelonephritis. CT chest, abdomen, and pelvis showed multiple cavitary lesions bilaterally in lung lobes concerning for septic emboli (Figure 1). At the time, the patient was presumed to have pyelonephritis complicated by gram negative bacteremia resulting in native valve endocarditis and septic emboli. Transthoracic echocardiogram showed normal ejection fraction at 57% and no vegetations. The patient was kept on broad spectrum antibiotics with unremitting fever. On hospital day five, blood cultures speciated to Fusobacterium Necrophorum. CT neck with contrast showed left pharyngitis with internal jugular thrombophlebitis (Figure 2). Diagnosis of Lemierre syndrome was made based on the clinical picture and CT neck findings. Antibiotic regimen was switched to intravenous Ampicillin / Sulbactam. Fevers subsided and the patient was discharged with a 6-week Amoxicillin / Clavulanic acid prescription.
Discussion: Lemierre syndrome, also known as jugular vein suppurative thrombophlebitis, is a rare oropharyngeal disease commonly caused by infection with the anaerobic Fusobacterium Necrophorum. (1) Clinical manifestations classically begin with fever and rigors one to two weeks following oropharyngeal infection. (1) Our patient was treated with recommended therapy of β-lactamase-resistant antibiotics with anaerobic activity, due to some reports of β-Lactamase production by some F. necrophorum. (2) F. necrophorum appears to be responsible for 10% of all throat infections. (3) Early detection is challenging due to the wide differential diagnosis for sore throat as seen in this patient with negative throat swab. Culturing Fusobacterium requires a special medium, our laboratory does not routinely use. As a result, the patient’s throat culture would not have shown Fusobacterium. This raises the question of the utility of testing for Fusobacterium given the rare, but severe complications that can result. Bank and colleagues. (4) conducted a cost-effectiveness analysis of testing cases of pharyngitis in the high-risk age group (15–24 years) with throat swabs to detect F. necrophorum and treating positive results with antibiotics. They found that, because of the high cost burden of Lemierre syndrome and peritonsillar abscess, it would take only 26% in case reduction for testing for Fusobacterium to be cost-effective. (4)
Conclusions: Though Lemierre syndrome is a rare condition in the post-antibiotic era, there have been increasing diagnoses in recent years. It is plausible that giving treatment for throat cultures positive for F. necrophorum would lead to a reduction in incidence of Lemierre syndrome. Throat swabs from 15-24 year-olds would need to be taken with the initial sore throat, because once thrombophlebitis has occurred, the infection is largely intravascular and there is rarely any pharyngeal exudate. (5) This requires further investigation with a prospective study to be deemed an effective public health measure.