Background: De-implementation of low-value services remains a challenge in healthcare. Research has shown that Choosing Wisely recommendations are ineffective in reducing low value care alone, and more robust interventions are needed. Additionally, most of the published efforts of reducing unnecessary inpatient services are done in smaller settings within a single hospital. Furthermore, initiatives in resource limited settings, such as safety net health systems are lacking in literature.
Purpose: In this quality improvement initiative, we proposed a multifaceted intervention to reduce 5 low-value services across 10 hospitals.
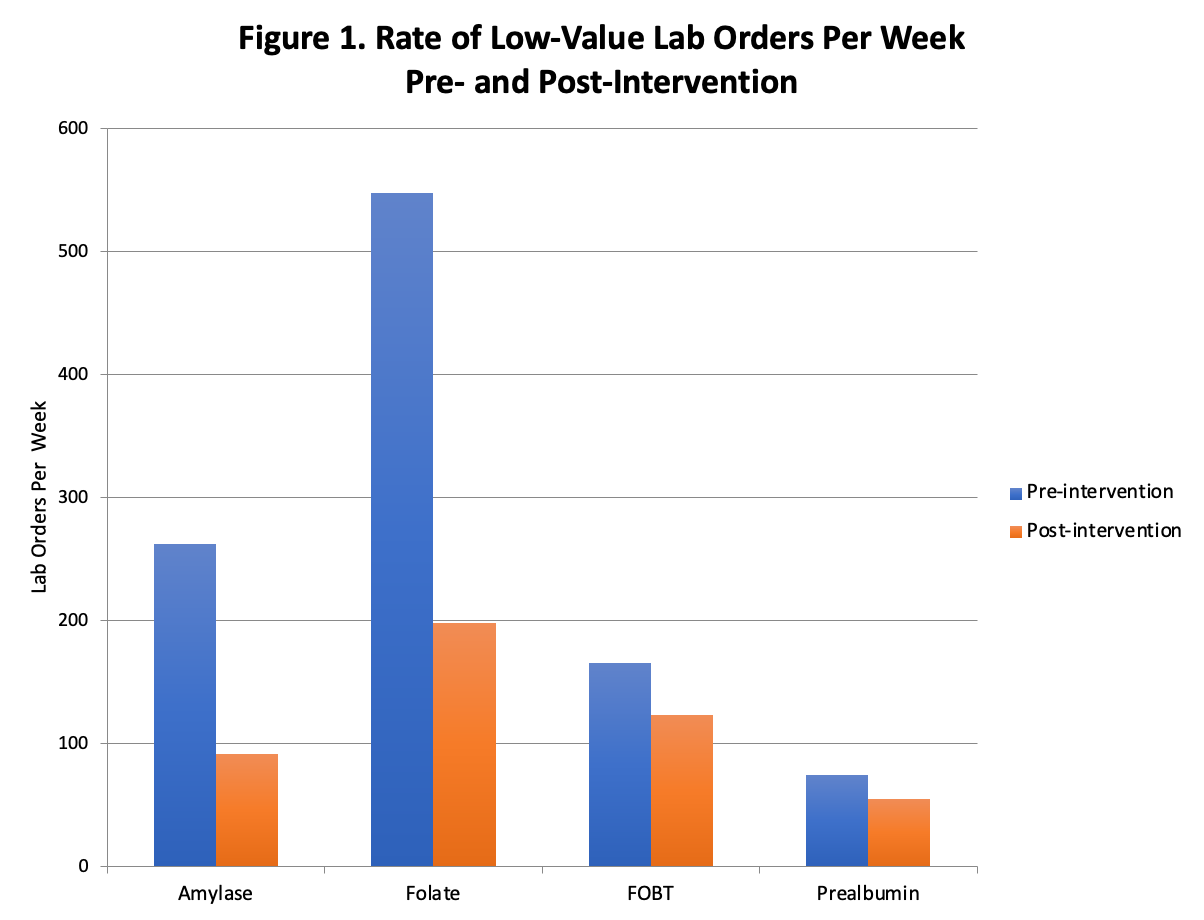
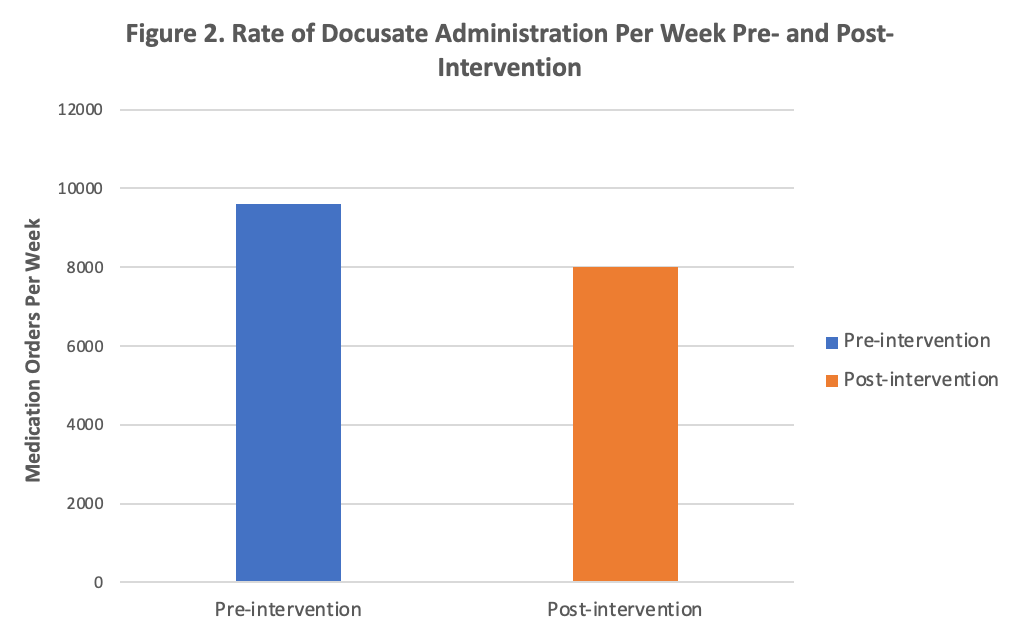
Description: In an urban, safety net health system, we implemented a multifaceted intervention which included (1) a multidisciplinary, multi-hospital development of consensus recommendations on 5 low-value care practices, (2) email and newsletter dissemination to site leadership and frontline staff, and (3) a “nudge” non-intrusive intervention on electronic health record orders. Our program targeted five inpatient targets (4 laboratory tests and 1 medication): docusate, amylase, folate (red blood cell and serum), prealbumin, and fecal occult blood test (FOBT).Pre-intervention data was collected from August 1, 2019 to November 20, 2019 and compared to post-intervention data from November 21, 2019 to July 1, 2020. Utilization decreased significantly on all 5 services [Figure 1, 2]: Docusate 9593 orders/week to 7993 orders/week (p <0.001), amylase 262 orders/week to 91 orders/week (p <0.001 ), folate (red blood cell and serum) 547 orders/week to 198 orders/week (p <0.001), prealbumin 74 orders/week to 55 orders/week (p= 0.002), FOBT 165 orders/week to 123 orders/week (p <0.001). Estimated charge cost savings for amylase, folate, prealbumin, and FOBT was $1,173,162.21 over one year.
Conclusions: By implementing this multifaceted intervention, we demonstrated significant reduction of 5 low-value services across 10 hospitals in a safety net health system. The intervention was centered around a nonintrusive “nudge,” effectively altering clinician ordering behavior without limiting ordering options, or introducing an intrusive hard stop or best practice advisory “pop up,” which can contribute to clinician burnout. This initiative demonstrated a low effort, high impact intervention that can serve as a model for other institutions, particularly low-resource settings, to reduce unnecessary testing and treatment without needlessly burdening clinicians.