Background: Gastric Point-of-Care Ultrasound (POCUS), has been validated for perioperative pulmonary aspiration risk reduction, but data on medical inpatients is lacking (1). Inpatients often have multiple risk factors for delayed gastric emptying, but may need urgent surgery or procedures. According to the American Society of Anesthesiologists (ASA), a fasting period of 2, 6, and 8 hours is recommended after ingestion of clear liquids, a light meal, and fried/fatty foods, respectively (2). However, the ASA admits that following these guidelines does not guarantee complete gastric emptying (2). Methadone, which is commonly used to treat opiate use disorder, is a drug known to increase risk for delayed gastric emptying (3). Patients taking methadone are often medically underserved and under-studied (4). We sought to use gastric POCUS to evaluate medical inpatients prescribed methadone in order to determine a perioperative aspiration risk assessment.
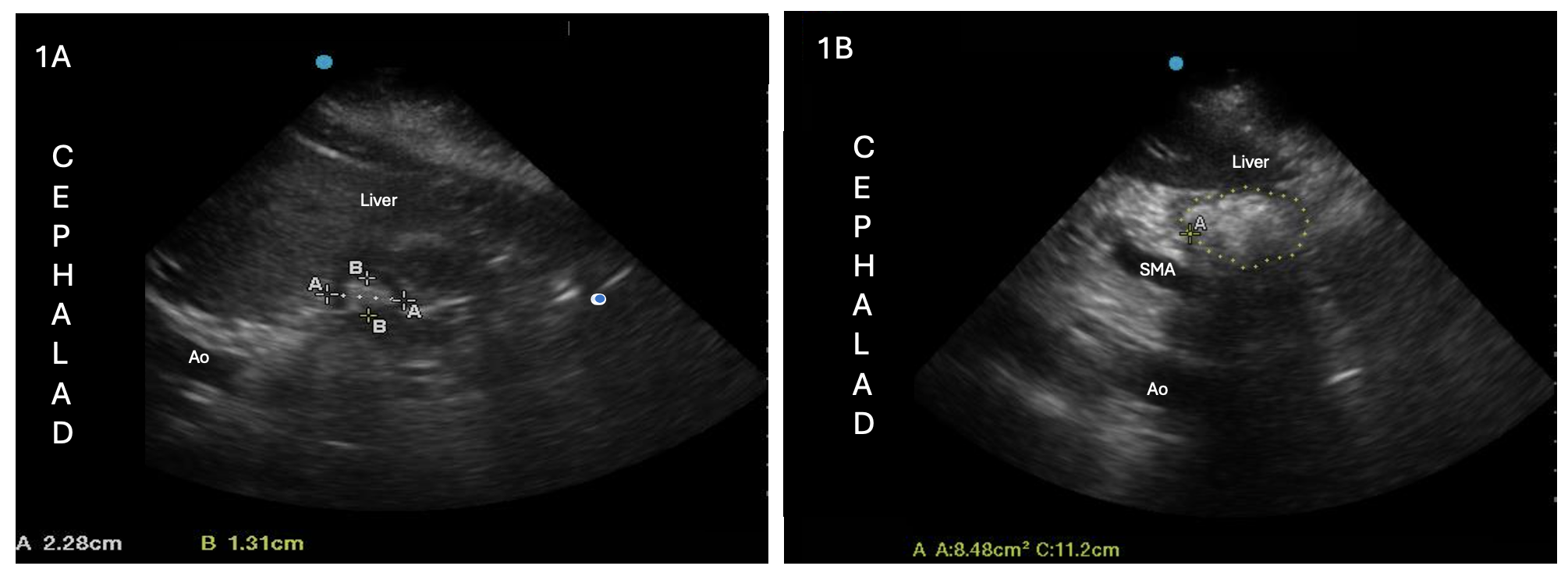
Methods: In this prospective observational cohort study (IRB # 2024-15822, enrollment dates 6/7/24-11/15/24), hospitalized patients prescribed methadone were asked to recall their consumption in the prior 14 hours, including meals, liquids, and snacks. Subjects were scanned before breakfast after an overnight fast regardless of pre-procedure status. Each subject was scanned 4 times: 2 in the supine position, and 2 in the right-lateral decubitus (RLD) position. Once the gastric antrum was identified with the liver and aorta in view, the operator completed measurements: cranial-caudal (CC) distance, anterior-posterior (AP) distance, and antral free-trace cross sectional area (CSA). These were repeated twice in each position (supine vs. RLD) and averaged. A blinded expert read each scan as either empty, liquid, or solid. Patient characteristics were compared using unpaired t-tests and Fisher’s exact test.
Results: Of the 12 patients, 8 (66.7%) had non-empty stomachs on gastric ultrasound after an overnight fast (Figure 1). Of those 8 patients, 7 were interpreted as solid-filled stomachs, and 1 was rated as having liquid contents (liquid volume/patient weight of 2.10 mL/kg, which is deemed as “unsafe” by the Perlas Equation (1)). The 4 patients with empty stomachs had an average time since last meal of 17.56 hours (95% CI 9.64 – 25.48), compared to 11.88 hours (10.24 – 13.52) in the 8 non-empty stomachs. Those with non-empty stomachs were more often older, less fasting time, with higher doses and longer duration of methadone, and higher percent Hispanic (Table 1). Empty subjects had comparatively smaller mean supine and RLD antral CSAs of 3.93 cm2 (2.16 – 5.70) and 6.22 cm2 (4.96 – 7.48), respectively, while non-empty subjects had mean supine and RLD antral CSAs of 8.59 cm2 (5.467 – 11.72) and 10.4 cm2 (5.59 – 15.21), respectively.
Conclusions: In hospitalized patients prescribed methadone, two-thirds of patients had non-empty stomachs on gastric POCUS after at least an 8-hour fasting period, suggesting that an 8-hour fast could be insufficient for inpatients prescribed methadone if they are planned for a surgery or procedure. This result has significant implications for the anesthesiology plan in terms of reducing perioperative pulmonary aspiration and highlights the utility of gastric POCUS as a pre-operative tool for risk stratification. Further work is needed to identify risk factors for subclinical delayed gastric emptying in patients prescribed methadone for opiate use disorder and how to safely manage these patients in the perioperative period.