Background:
Most patients in the ICU obtain excellent glycemic control with the use of an insulin drip protocol. How best to transition patients to a subcutaneous regimen and maintain adequate glycemic control is less well established. We evaluated how effectively glycemic control was maintained during transition from IV to subcutaneous insulin in 2 ICUs at an academic hospital to assess the need for a transition protocol.
Methods:
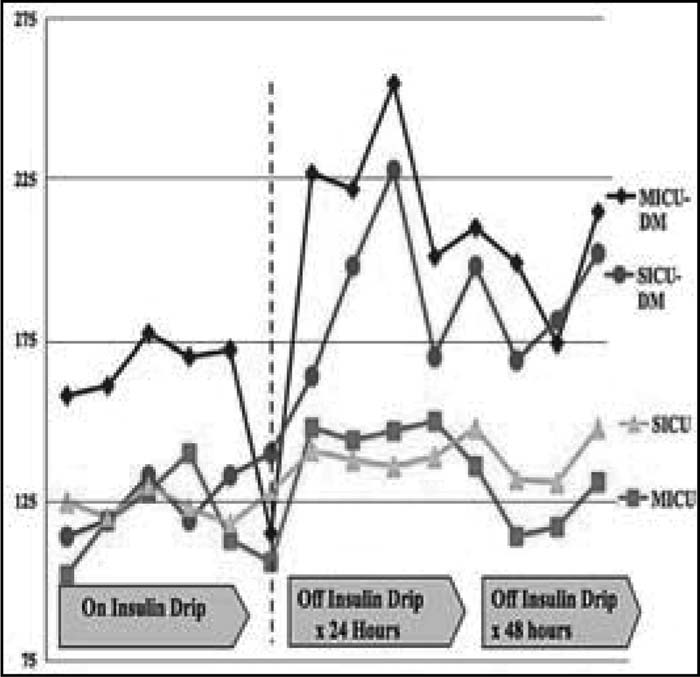
Data from 24 SICU and 17 MICU patients placed on an insulin drip for more than 24 hours were prospectively collected. Patients were excluded if they were on a drip for less than 24 hours or did not remain in the hospital for more than 48 hours after stopping the drip because of death or discharge. SICU insulin orders were written by a single pharmacist whereas, MICU insulin orders were written by the resident on duty. Glucose values were collected 6 hours prior and 48 hours after stopping insulin infusion, and information was gathered on insulin dosing, nutritional requirements, Hgb A1c, and a medical history of diabetes.
Results:
Of the 17 MICU patients, the average glucose on the drip was 158 mg/dL for diabetic patients (n = 11) and 117 mg/dL for 6 nondiabetic patients (P = .002). After transferring off the drip, diabetics had an average blood sugar in the first 48 hours of 212 mg/dL and nondiabetics an average blood sugar of 136 mg/dL (P < .001). Of the 24 SICU patients, the average blood sugar on the drip was 128 mg/dL for diabetic patients (n = 10) and 125 mg/dL for nondiabetic patients (n = 14; P < .001). After transferring to a subcutaneous regimen, the average blood sugar in the first 24 hours was 190 mg/dL for diabetic patients and 139 mg/dL for nondiabetic patients (P < .001). There was a combined total of 22 hyperglycemic events (>300 mg/dL) and 5 hypoglycemic events (<70 mg/dL) in the diabetic patients. There were 2 hypoglycemic events in the nondiabetics. The average time between stopping the drip and administering the first dose of basal insulin was 7 hours for both MICU and SICU patients.
Conclusions:
After the transition off infusion insulin, we noted underdosing of insulin, failure to provide subcutaneous insulin before the insulin drip was stopped, and resultant poor glycemic control. Nondiabetic patients maintained adequate glycemic control despite the lack of an appropriate care plan for their hyperglycemia. These preliminary data demonstrate the need for an insulin transition protocol.
Author Disclosure:
G. Maynard, Sanofi Aventis, honorarium speaker; P. Ramos, none; D. Childers, none.