Background: Hospital-acquired delirium is serious, leading to increased falls, pressure ulcers, length of stay (LOS), cost, patient institutionalization, and patient and caregiver distress. In addition, it is associated with mortality rates as high as 35-40% within one year in older patients who develop delirium. Because hospital-acquired delirium is often under-recognized and prevention and treatment involves multi-disciplinary care coordination, comprehensive programs to decrease delirium are often lacking.
Purpose: To develop and implement a multi-disciplinary pathway to prevent and treat delirium at a large, tertiary care urban hospital.
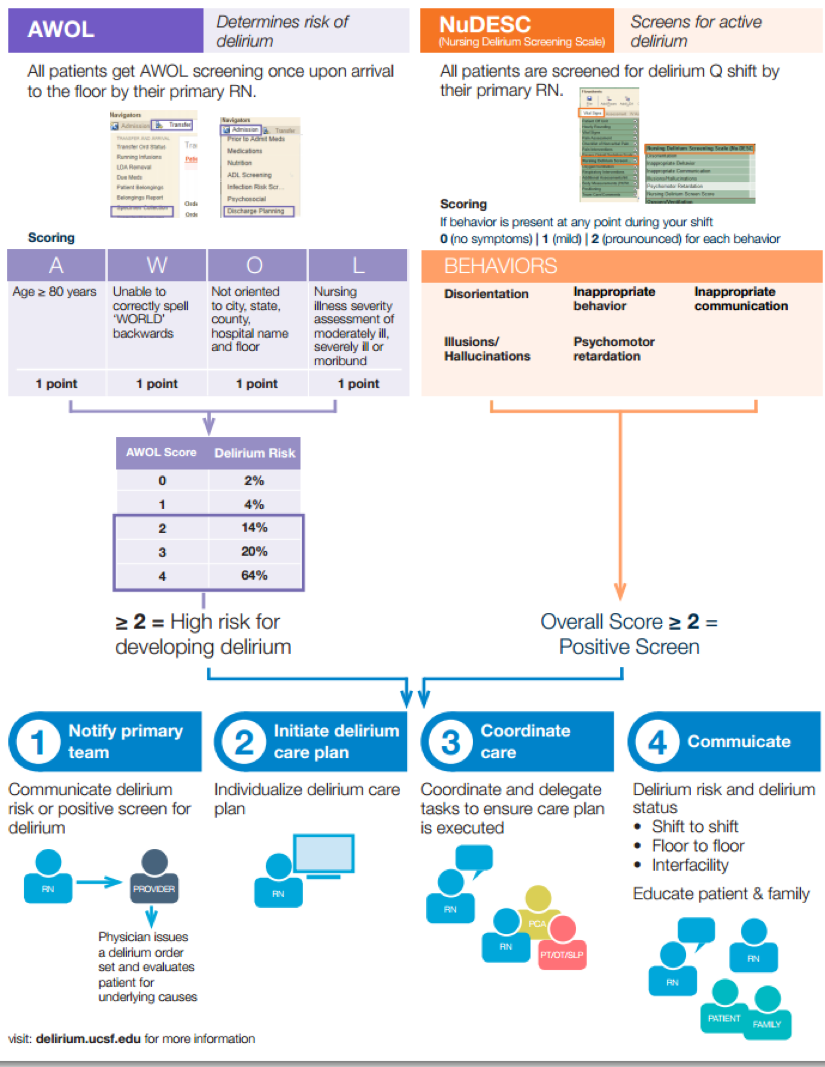
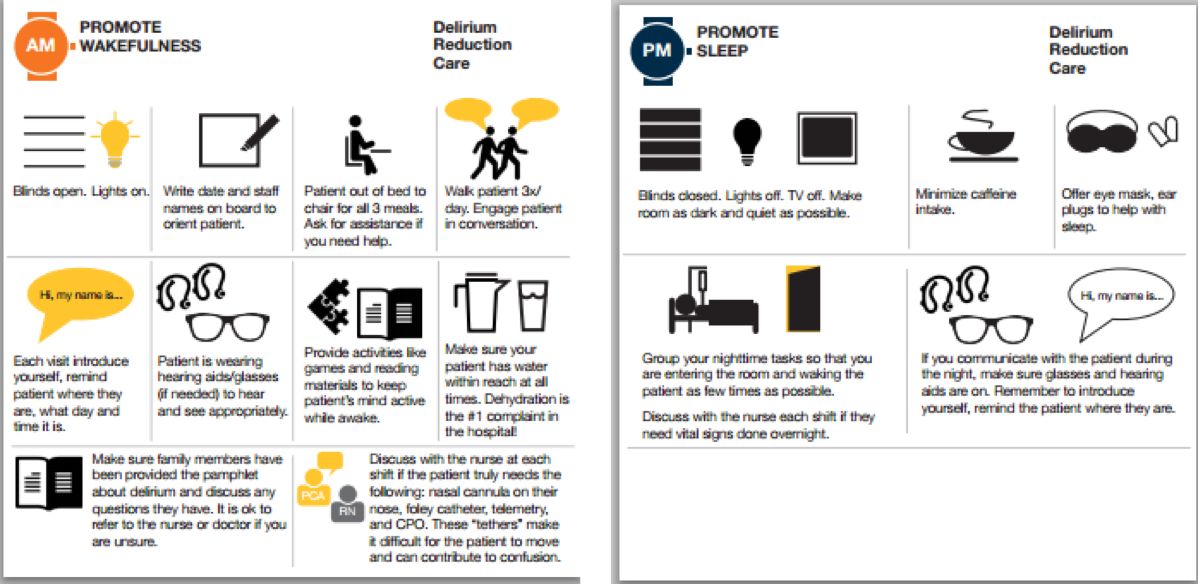
Description: A team consisting of a geriatrician, hospitalist, neurologist, and service design experts created a comprehensive, evidence-based delirium screening, prevention, and treatment pathway (Figure 1). Nurses screen all patients for delirium risk on admission using a previously validated screening tool. Patients who screen at higher risk for developing hospital-acquired delirium are placed on a non-pharmacologic protocol for delirium reduction care (Figure 2) after nurses contact the physician caring for the patient. The non-pharmacologic delirium care protocol includes mechanisms to promote wakefulness and mobility during the day and promote sleep at night.
Patients are screened for delirium on each nursing shift, and physicians are notified if their patients are identified as being delirious. In addition to activating the non-pharmacologic delirium protocol, physicians evaluate patients for the underlying cause(s) of delirium, and pharmacists perform a comprehensive review of the inpatient medication list and discontinue potential offending medications.
The pathway was implemented on the hospital medicine service in January 2017. As of September 2017, nursing compliance with AWOL screening is > 90%, compliance with Nu-Desc screening is > 80%, and physician activated delirium order set compliance within 12 hours of a positive delirium screen is > 60%. LOS in patients with delirium on medicine units decreased by 1.1 days, or a 10% decrease.
Conclusions: The creation of a comprehensive, multi-disciplinary delirium prevention and treatment pathway can lead to improvements in the care of patients who are at risk for delirium and who develop delirium in the hospital. Further study is needed to determine if improvements in LOS and cost are sustained, and if the pathway can impact other delirium associated morbidities and mortality.