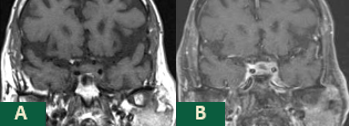
Case Presentation: A 75-year-old male presented to our institution with lethargy and unremitting headache of several weeks duration. His history was significant for squamous cell carcinoma of the lung status post lobectomy with recurrence 4 years later being treated with palliative radiation, chronic obstructive pulmonary disease (COPD), and hypertension. He described his headache as daily, aching, non-radiating retroorbital pain that progressively worsened over several weeks and did not respond to Butalbital/Acetaminophen/Caffeine and oxycodone. Pain was not exacerbated by light, sound, or eye movement. MRI of the brain 1 month prior was negative for metastases. On examination, vitals were normal. The patient was somnolent but oriented x 3 and able to answer all questions appropriately. Initial neurological examination was unremarkable. However, serial neurological examinations revealed progressively worsening left ptosis and dysconjugate gaze with preserved visual fields. Laboratory studies were significant for hyponatremia, hypocortisolemia, hypothyroidism and low follicle stimulating hormone (FSH) and testosterone levels consistent with panhypopituitarism. Repeat MRI of the brain with pituitary protocol was consistent with metastases to the anterior pituitary and infundibulum with extension into the left cavernous sinus. Treatment was initiated with steroids and thyroid replacement with improvement in the patient’s lethargy and hyponatremia. His headache was minimally improved with intravenous hydromorphone but did improve with the addition of valproic acid and gabapentin. Neurosurgery performed transphenoidal biopsy with debulking with histology confirming metastatic squamous cell carcinoma of the lung. He tolerated surgery well but continued to have persistent headaches. Repeat MRI of the brain two weeks following surgery revealed mild progression of disease in the pituitary and infundibulum, which will be treated with adjuvant radiation.
Discussion: This case is an example of an unusual presentation of metastatic squamous cell carcinoma of the lung to the pituitary gland highlighted by isolated anterior involvement with panhypopituitarism, rapid progression, and persistent, refractory retroorbital pain. There should remain high clinical suspicion for patients with known malignancy who develop similar symptoms to those seen in our patient despite recent negative imaging due to the rapidity of disease progression. MRI of the brain should be ordered with pituitary protocol for optimal visualization of the pituitary gland. Control of pain secondary to pituitary metastases may be difficult with opioids alone, but anti-epileptics may provide some degree of analgesia given the neuropathic characteristics of the pain associated with these tumors.
Conclusions: Although several malignancies are known to commonly metastasize to the brain, metastatic disease localized to the pituitary gland is rare. Metastases from breast and lung primary malignancies are the most frequently described. Pituitary metastases are typically asymptomatic. However, they may progress rapidly and control of the pain associated with extensive involvement of these tumors may be difficult to accomplish.