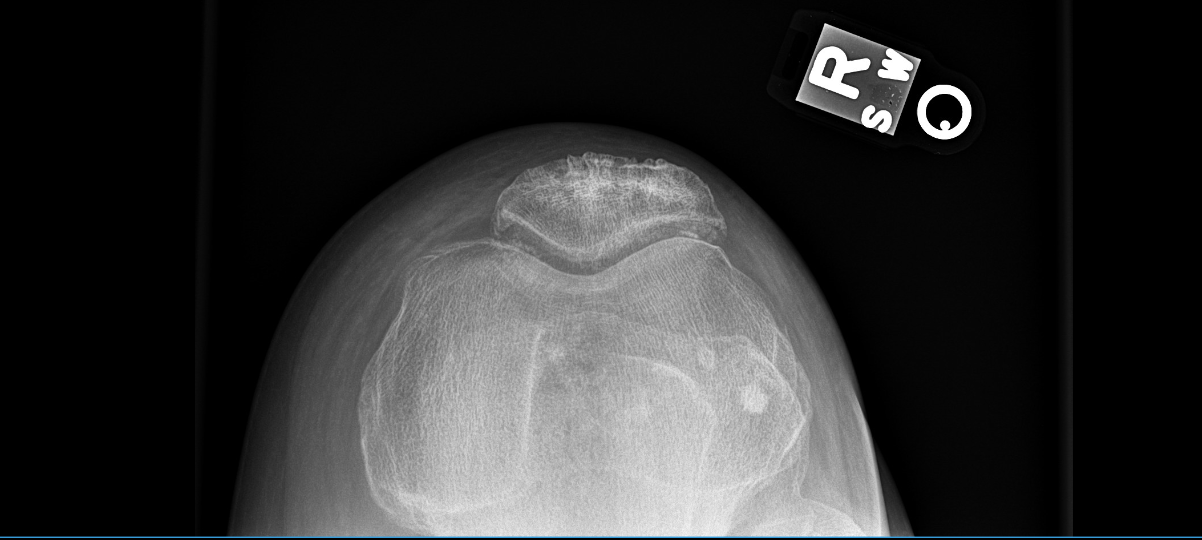
Case Presentation: A 60-year old gentleman with past medical history of liver transplant 5 years ago presented to the hospital with acute onset of right-sided knee pain. For his immunosuppressive regimen, he took 2 mg/day of tacrolimus. However, the patient reported noncompliance with his outpatient follow-up. His social history was negative for excessive alcohol use and high-protein diet. His physical examination was significant for right knee warmth, swelling, and erythema with tenderness upon palpation. Labs indicated normal white blood cell count, normal creatinine at 0.81 mg/dl, tacrolimus at 9.3 ng/ml, uric acid at 6.1 mg/dl, and elevated C-reactive protein at 18.1 mg/L. Synovial fluid analysis showed 27,000 nucleated cells with differential of >90% neutrophils and intracellular monosodium urate crystals. Fluid cultures were negative and ruled out septic arthritis. This patient was diagnosed with acute gouty arthritis, and the patient was administered colchicine for three days. His tacrolimus dosage was decreased from 2 mg/day to 1 mg/day. With treatment, the patient’s symptoms resolved, and he was continued on the adjusted dose of tacrolimus with outpatient follow-up
Discussion: For tacrolimus, the effect on uric acid levels is not as well established compared to cyclosporine’s effect. Hyperuricemia has been reported in patients taking tacrolimus, but there have been only a few reported cases of gout. The reason for the discrepancy between cyclosporine-induced and tacrolimus-induced gout may be that cyclosporine can promote increased uric acid reabsorption in the proximal tubules and decreased GFR following afferent arteriole vasoconstriction, whereas tacrolimus is only known to reduce the excretion of uric acid. Hyperuricemia can be seen in 14-47% of liver transplant patients, predominantly due to accompanying decreased renal function. In these liver transplant patients, tacrolimus has emerged as the go-to maintenance regimen over cyclosporine due to data indicating increased patient and graft survival and decreased acute rejection. Therapeutic levels of tacrolimus remain controversial. They need to be individually catered to patients and their specific comorbidities and functional status. Current guidelines indicate the following: in the first 4-6 weeks following a liver transplant, the trough levels of 10-15 ng/ml are recommended and 5-10 ng/ml thereafter to maintain a balance between nephrotoxicity and acute rejection. In the context of this patient (tacrolimus level at 9.3 ng/ml), his tacrolimus levels are on the upper range of target trough levels and may have been significant enough to cause tubular dysfunction. Since tacrolimus undergoes liver metabolism, the elevated tacrolimus levels in a patient with liver transplant combined with noncompliance with outpatient follow-up may have contributed to hyperuricemia and the development of gout.
Conclusions: Every clinician should be aware of potential side effects of calcineurin inhibitors such as cyclosporine and tacrolimus. Their effects should be monitored during initial hospitalization, and expert opinion should be sought for dose adjustments. Also, the patients should be advised about the importance of regular outpatient follow-up to monitor drug levels and avoid the potential of drug-induced toxicities.