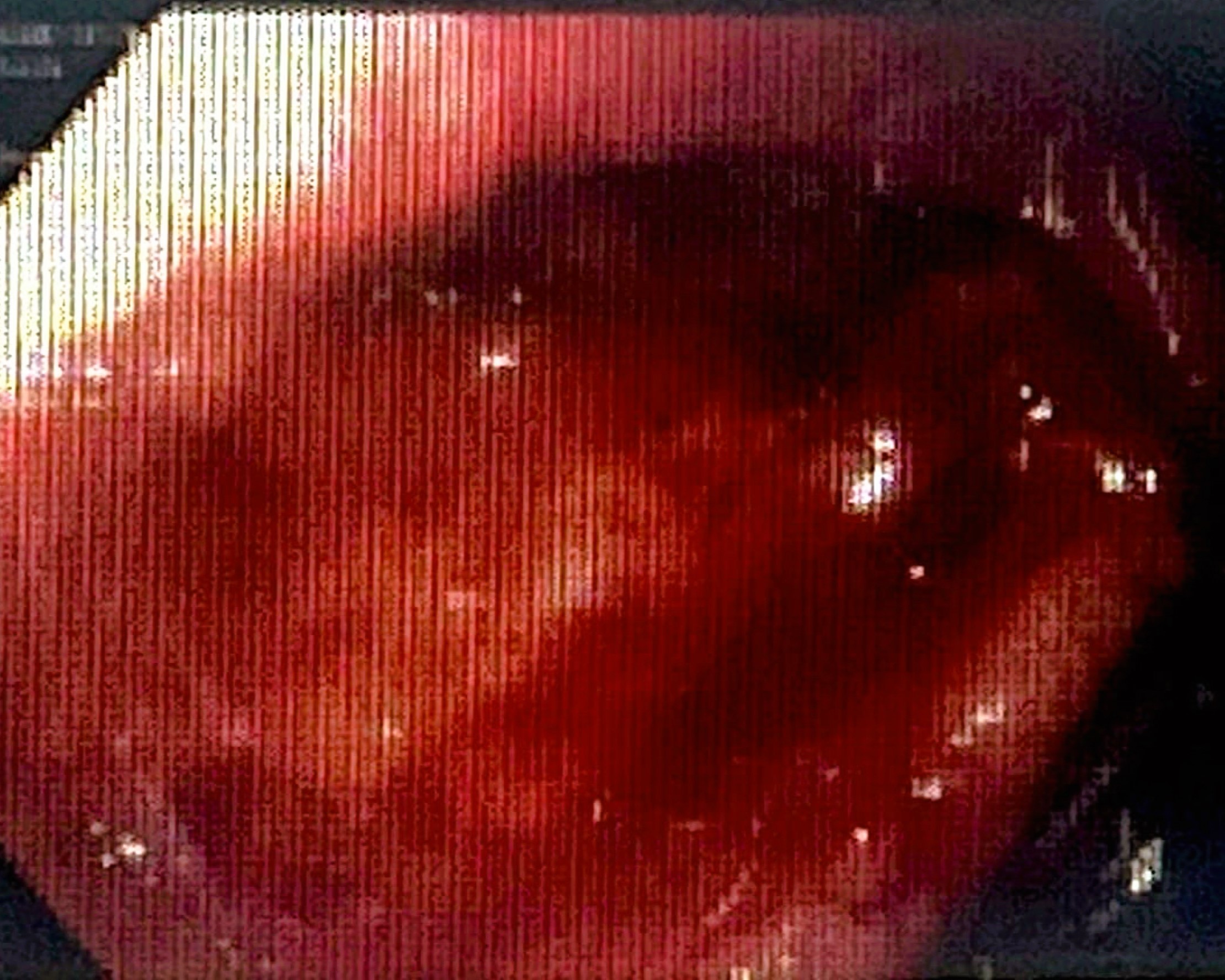
Case Presentation: We present the case of a 53-year-old male with hypertension presented to the emergency department with progressively worsening of altered mental status. Family reported fatigue, poor appetite, confusion, slow responses, social withdrawal, missing work. Patient experienced slowing of thought process, soft speech, déjà vu (events replaying over and over again in mind). He also had chronic dyspepsia and a recent episode severe chest pain, ruled out acute coronary syndrome. On initial encounter, he was slow to answer questions but provided contextual answers and followed commands with repeated explanations. Physical exam and brain imaging were unremarkable. Lab test showed mild anemia and EEG were normal. During admission, patient experienced melena and dizziness, leading to intubation due to encephalopathy. Upper gastrointestinal endoscopy identified a bleeding duodenal ulcer. Hemostasis was achieved with epinephrine injection. Post-extubating, he had dysphagia with continued mood disturbances. Modified barium swallow study ruled out vocal cord injury. Gastric biopsies result confirmed H. pylori infection, quadruple therapy was initiated. Psychiatry evaluated the patient, diagnosing catatonic mutism for which Lorazepam was initiated. He completed 14-day course of quadruple therapy. His dysphagia and energy levelssignificantly improved. Lorazepam was subsequently tapered off, and the patient was discharged on fluoxetine and pantoprazole. Follow up stool antigen study six weeks post-treatment confirmed eradication of H. pylori.
Discussion: The gut-brain axis involves a complex network of biochemical and neural pathways that allow for communication and interaction between the gut and the brain. H. pylori infection can lead to gastrointestinal symptoms such as inflammation, increased permeability of the intestinal lining, and alterations in gut microbiota composition. This dysbiosis in the gut microbiota may influence the production and metabolism of neurotransmitters such as serotonin, dopamine, and GABA which play key roles in regulating mood. Imbalances in these neurotransmitters have been linked to depression. Furthermore, certain bacteria in the gut produce short-chain fatty acids (SCFAs), which have been shown to have neuroprotective and anti-inflammatory effects. Disruptions in the gut microbiota caused by H. pylori infection can alter the production of these beneficial metabolites, potentially impacting brain function and mental health.
Conclusions: It is worth noting that this case highlights the psychiatric manifestations and neurological consequences associated with H. pylori infection, such as depression, altered mental status, and catatonic symptoms. Prompt recognition and appropriate management, including both the treatment of H. pylori infection and psychiatric interventions, were crucial in achieving improvement in the patient’s overall condition. From literature review, many studies prove H pylori can cause Depression, Alzheimer’s dementia, Parkinson’s disease and other inflammatory disease including ischemic stroke. There is one case report mentioning H pylori induced catatonia. The association between mental health and gut health is a rapidly growing field of research that holds great promise for advancements in gastroenterology and beyond. The case report also prompts discussions about the potential use of microbiome repletion strategies in the context of mental health and gastrointestinal disorders.