Background: Despite the current focus on developing handoff training curricula to improve patient safety, rigorous assessments of handoffs remain scarce. Immersive simulations allow for the evaluation of communication skills, but few specifically account for common external threats to effective handoff performance. Our aim was to investigate the effects of these interruptions in an educational handoff simulation.
Methods: Entering PGY1 interns at a single academic medical center were required to complete a handoff simulation exercise. Participating interns were instructed to verbally hand off a panel of three patients to trained receivers using a standardized written sign-out document. Interns were randomized to three simulation conditions: (1) an uninterrupted handoff, (2) a handoff with routine hospital noise (70-91 dB), or (3) a handoff with hospital noise and two pager interruptions sent to a trained receiver. Receivers evaluated participants using an evidence-based checklist of handoff best practices and a validated handoff mini-CEX instrument. Descriptive statistical methods were used to summarize the data.
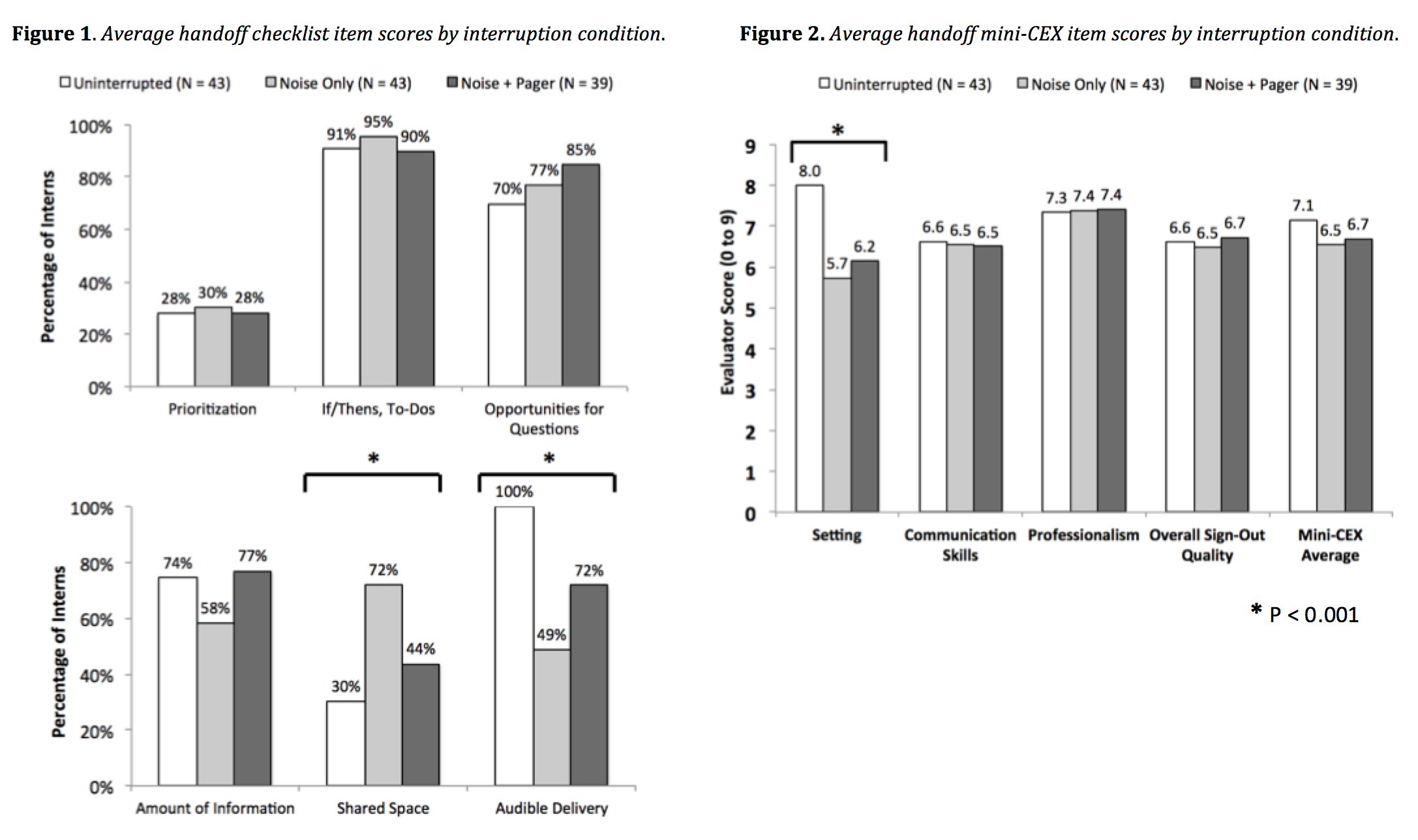
Results: Nearly all (125/127 [98.4%]) eligible participants completed the simulations. Out of 125 simulations, 43 (34.4%) included ambient noise only, 39/125 (31.2%) included both noise and pages, and 43/125 (34.4%) were uninterrupted. Participants receiving hospital noise only were more likely to effectively share the written sign-out document (71.1% compared to 30.2% uninterrupted and 43.6% noise/pages, p < 0.001). Interns receiving either interruption (noise with or without pages) were less likely to be heard adequately (48.8% noise and 71.8% noise/pages compared to 100.0% uninterrupted, p < 0.001). Additionally, though no significant differences were found in communication skills, professionalism, or overall quality, though interns receiving either interruption condition scored lower on establishing an appropriate handoff setting (5.7 ± 2.3 noise and 6.2 ± 1.8 noise/pages compared to 8.0 ± 0.8 uninterrupted, p < 0.001). In handoffs with pages, most participants recovered effectively from interruptions (31/39, 84.2%) and avoided side conversations (35/38, 89.7%). On a follow-up survey administered one month later, 100/125 (80.0%) interns reported conducting better handoffs in practice as a result of the simulation.
Conclusions: While common hospital interruptions created non-ideal circumstances for effective communication, handoff performance was similar across all conditions. However, most interns were able to recover effectively from pages and avoid side conversations, and participants exposed to hospital noise used the written sign-out form more effectively. This finding underscores the importance of standardized templates and protocols in avoiding handoff errors.