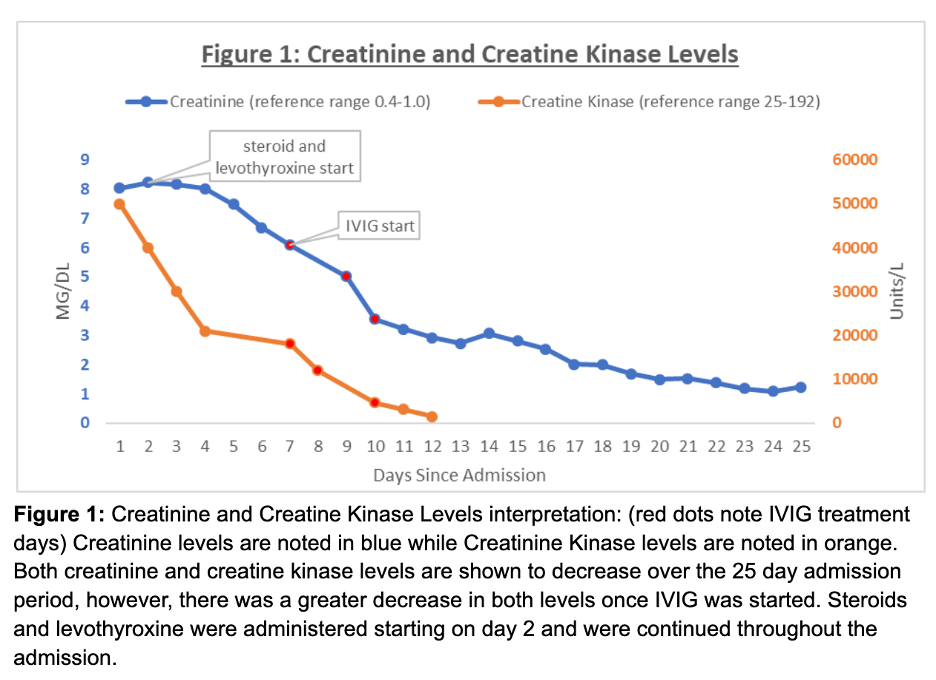
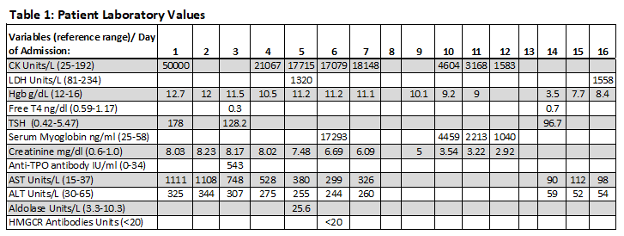
Case Presentation: This abstract discusses the inpatient care of a 74 year-old female who had three hospital admissions throughout 2022 with a detailed focus on the second admission. According to the patient’s discharge summary from her first admission, she was diagnosed with severe rhabdomyolysis (secondary to statin use) and acute renal failure requiring outpatient hemodialysis. She was positive for COVID19 approximately two weeks before her first admission and presented with progressive generalized weakness, body ache, dyspnea on exertion, fever, chills, and oliguria. The patient stopped her statin medication once hospitalized. Hemodialysis was discontinued approximately three months after discharge from first hospitalization due to significant improvement in renal function. A thyroid stimulating hormone (TSH) level was never checked during this hospital admission and the patient reported no previous history of thyroid disease.One month after stopping hemodialysis, the patient had her second admission with similar symptoms except for oliguria and fever. Her initial creatinine kinase was greater than 50,000 U/L with a TSH level of 177.95 mlU/L. The patient was started on 100mg IV levothyroxine daily and 100mg IV hydrocortisone every 8 hours. With the utilization of risk-benefit analysis, a muscle biopsy was recommended to assess for myositis. The patient was started on intravenous immunoglobulin (IVIG) for four days and the biopsy was negative for myositis. As shown in Figure 1, the creatinine and creatine kinase levels dramatically decreased after administration of IVIG. It is important to note that the patient started to feel improvement of her fatigue and weakness on day 11 of hospital stay. Table 2 shows pertinent laboratory results. The patient was readmitted to the hospital for 11 more days due to severe blood loss from the biopsy site and altered mental status. The patient’s initial hemoglobin was 3.7 and CT imaging revealed a 12x3x6 cm intramuscular hematoma. She received ICU care with appropriate blood transfusions and was discharged after being able to ambulate with a walker and baseline mental status.
Discussion: This patient never reported having thyroid disease prior to her second hospitalization in 2022. One theory proposed from this case study is an increased risk of developing Hashimoto’s Thyroiditis (HT) after COVID19 infection. There is growing evidence associating viral infections with HT. Two common theories are molecular mimicry and the bystander effect.Screening for hypothyroidism remains to be controversial when looking at recommendations by expert groups. This case study suggests more investigation into guidelines regarding screening patients for thyroid disease, especially during hospitalization.Starting IVIG in this patient was done due to high clinical suspicion for autoimmune myositis. There are minimal studies utilizing IVIG for HT causing rhabdomyolysis. This case study reveals a possible alternative treatment for severe autoimmune thyroiditis if not immediately responsive to thyroid hormone.
Conclusions: This case study represents another contribution to scientific literature towards an association between HT, severe rhabdomyolysis, and COVID19. In these circumstances, physicians should consider ordering a TSH during hospital admissions with close outpatient follow up. This case study is unique due to the long duration and extreme severity of HT with rhabdomyolysis observed.