Background: Migraine headache (MHA) is a common pediatric illness with up to 75% of children experiencing an episode by the age of 15. Up to 58% of adult MHA patients have a psychiatric comorbidity (PC), but the percentage of children with MHA and PC is unknown. At Phoenix Children’s Hospital (PCH), migraine is one of the top 10 most common admitting diagnoses. In order to improve and standardize care for patients with MHA, a protocol was developed consisting of 4 steps; Step 1) fluids, anti-emetics and NSAIDS; Step 2) addition of Valproate; Step 3) addition of magnesium; and Step 4) addition of dihydroergotamine (DHE) in escalating doses until headache is aborted. Adult literature shows that MHA patients with PC have a poor response to standard MHA treatments and protocols. The purpose of this study was to determine the effect of presence of PC on response to standard therapy for pediatric MHA patients as predicted by use of medication, length of stay (LOS) and hospital readmission rate (RR).
Methods: Using the Pediatric Health Information System (PHIS) database, we performed a retrospective cohort study of patients admitted to PCH between 1/1/2010 and 6/30/2018 with ICD 9 and 10 codes for migraine as a principal diagnosis. Data was collected on patient demographics, psychiatric comorbidity, medication use, RR, and LOS. Comparison of patients with and without PC was done using the Fisher exact or Wilcoxon-rank sum tests, as appropriate for the data distribution.
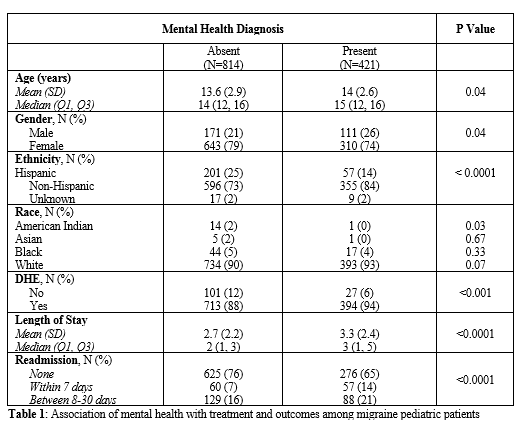
Results: Of 1235 total patients included in the study, 421 (34%) had PC. Demographic differences were noted between the two groups. The group with PC was more likely to be female, older in age and non-Hispanic. Patients in the group with PC were significantly more likely to receive DHE during their hospitalization (p=0.001), have longer mean length of stay, and higher readmission rates(p<0.0001) (Table1). No differences in the use of other medications was noted.
Conclusions: Pediatric patients with mental health disorders are more likely to fail traditional therapy when admitted for treatment of migraine, resulting in escalation of care and prolongation of the hospital stay. This may be due to several factors including shared serotonergic dysfunction between migraine and affective disorders and dysregulation of the hypothalamic pituitary adrenal axis noted in both depression and migraine. The treatment of MHA in the presence of PC requires an expanded approach to therapy to address these factors. Special attention is also required to ensure appropriate outpatient follow up for both headache and Psychiatric comorbidity. Further study is needed to aid in the development of a specialized Migraine headache protocol for children with psychiatric co-morbidity.