Background: Strategies to reverse the effect of warfarin, a vitamin K antagonist (VKA), may be necessary for patients who are actively bleeding, asymptomatic with markedly elevated INR values, or requiring urgent invasive procedures. The purpose of this quality improvement activity (QIA) was to evaluate adherence to the 2012 CHEST guidelines for use of vitamin K in the previously described clinical scenarios while simultaneously assessing the effect of vitamin K dose and route on change in INR.
Methods: This QIA was a multi-center retrospective chart review of inpatients requiring vitamin K for the reversal of INR (May-July 2015). The sample contained data from 9 hospitals within the North Shore–LIJ health system, including 5 tertiary and 4 community sites, with data on 180 random patients. The primary objective was to describe the change in INR (pre- to post-vitamin K) by vitamin K route of administration and dose. The secondary objective was to evaluate adherence to the 2012 CHEST guidelines for the use of vitamin K for VKA reversal. Descriptive statistics were used for vitamin K dose, frequency, and route of administration. The change in INR was compared using a Wilcoxon signed-rank test. The outcome of INR was log transformed to meet the standard assumptions of Gaussian residuals and equality of variance. Means and 95% confidence intervals (CI) were calculated on the log-scale.
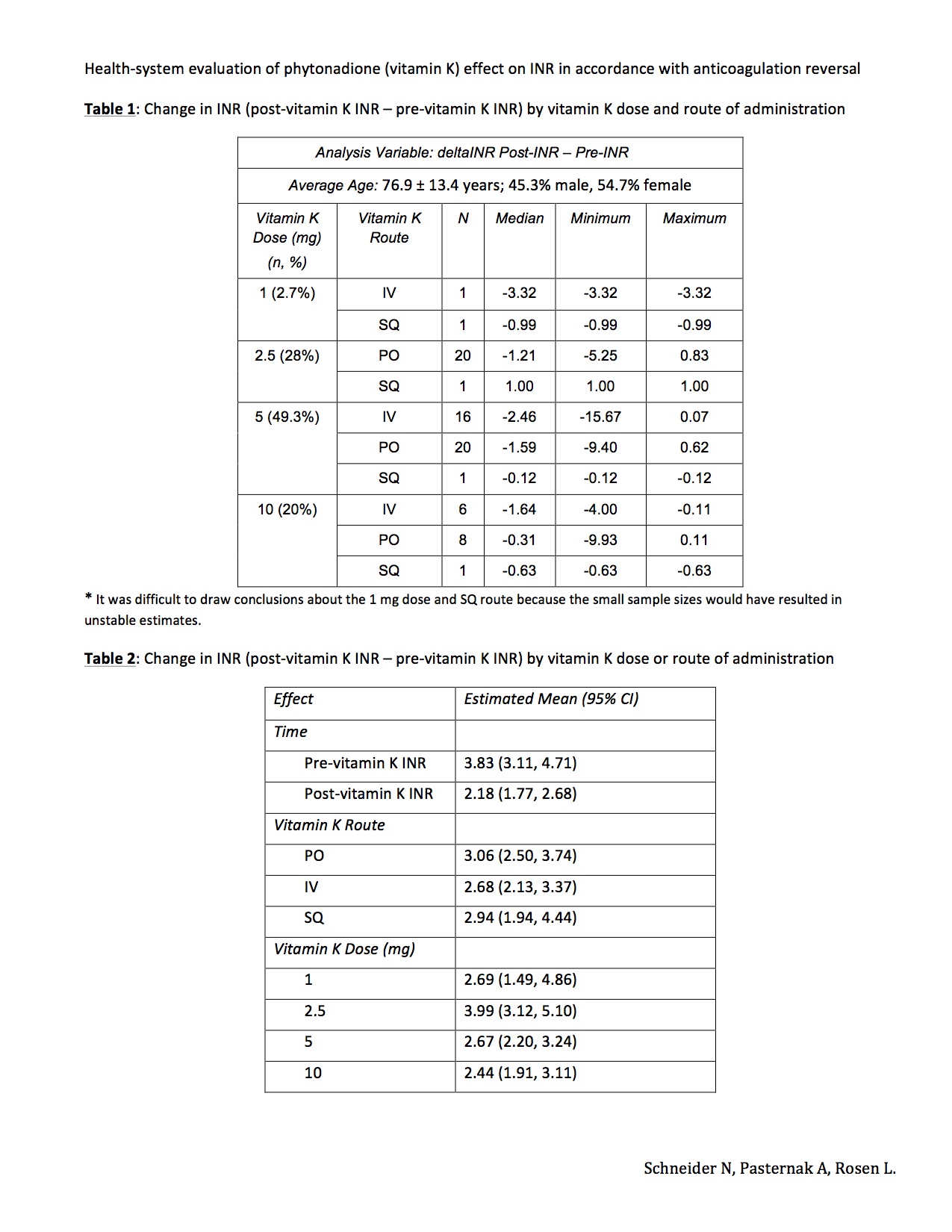
Results: The final sample included 180 patients, with 75 in the first subgroup evaluating vitamin K effect on INR change, and 158 in the second assessing adherence to the 2012 CHEST guidelines. In the first subgroup, the most common route of vitamin K was oral: 64%, followed by IV: 30.7% and SQ: 5.3%. The most frequent reasons for vitamin K use were elevated INR: 53.3%, peri-procedural reversal: 21.4%, and INR reversal with active bleeding: 18.7%. There was a significant difference between pre- and post-INR values (p<0.0001), with a decrease of -2.3 ± 3 (median: -1.2). Patients receiving 2.5 mg had higher pre- and post-vitamin K INR levels as compared to 5 and 10 mg (p<0.0018 and p<0.0014, respectively). However, after adjusting for dose, the change in INR by vitamin K route was not significant (p<0.5390). In the second subgroup, vitamin K was prescribed in the majority of patients for elevated INR: 47.5%, followed by active bleeding: 34.8% and peri-procedural reversal: 17.7%. Adherence to the CHEST 2012 guidelines by indications was 1.3%, 58.1%, and 46.5%, respectively.
Conclusions: Vitamin K decreased INR values but the magnitude of the effect did not depend on its dose or route. Overall adherence to the CHEST 2012 guidelines for reversal of VKA was low, especially in the elevated INR subgroup, indicating the need for education and re-evaluation of prescribing patterns. This QIA did not evaluate procedure types, urgency of reversal, or impact of transfusions. Larger studies are needed to confirm the results of this QIA.