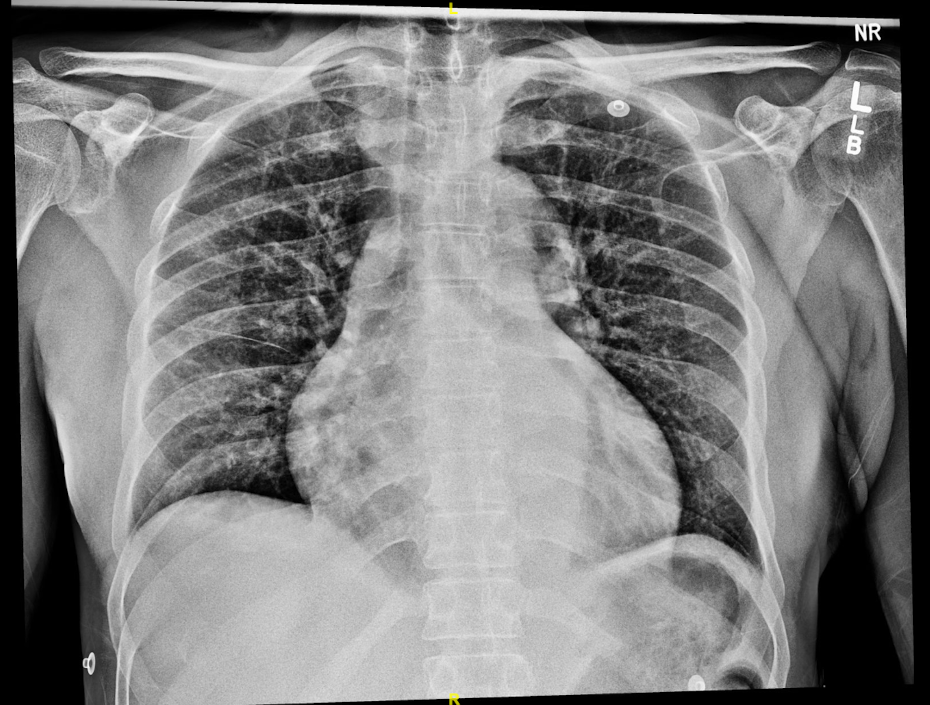
Case Presentation: A 52 year-old man with PMH of HIV presented with inguinal lymphadenopathy, intermittent abdominal pain, suprapubic fullness, fever and poor urine production for several days. Bladder catheterization yielded a large volume of bloody urine. The patient had not experienced hematuria previously and had no history of urinary retention, urgency, perineal or GU trauma. Patient’s lab findings were significant for lymphopenia and a CD4 count of 23 cells/µl. Subsequent tests for other infectious diseases including VZV, HSV, CMV, and toxoplasmosis were negative. A pelvic and abdominal CT was notable for diffuse retroperitoneal lymphadenopathy. IR-guided lymph node biopsy revealed presence of acid-fast bacilli (AFB) and blood cultures were positive for MAC. Patient was placed on HAART therapy which resulted in improvement of CD4 count from 23 cells/µl to 208 cells/µl in a span of 45 days. Simultaneously, anti-MAC pharmacotherapy with macrolide and ethambutol was initiated which resulted in overall clinical improvement and weight gain.
Discussion: Transmission of MAC is thought to be through inhalation and ingestion. Several studies have examined the effect of Proton Pump Inhibitors (PPI) on MAC and reported no significant effect on growth or GI dissemination. In contrast, Omeprazole use was associated with significant and more rapid growth of Mycobacterium Tuberculosis. Similar to TB, MAC also evades the innate immune system through inhibiting the fusion of phagosomes with acidified lysosomes in the infected alveolar or interstitial macrophages. Retroperitoneal and mesenteric lymphadenopathy is a common yet serious complication of disseminated MAC infection that is present in nearly 82% of AIDS patients. MAC mesenteric lymphadenopathy can lead to intussusception, hematochezia and bowel obstruction in children while it may present as diffuse abdominal pain in adults with an insidious onset. Several cases have been reported in which RL has caused duodenal obstruction due to extrinsic pressure onto the second and third segment of the duodenum leading to bilious or non-bilious vomiting. Due to engagement of the reticuloendothelial system, hepatosplenomegaly may also be present. Management of MAC consists of azithromycin or clarithromycin plus ethambutol or rifampin which should be continued at least 12 months after negative culture conversion.
Conclusions: Intermittent fever and lymphadenopathy are among some of the common manifestations of various malignancies including lymphoma. Retroperitoneal lymphadenopathy (RL) is often seen in cancers and is associated with poor prognosis. RL in AIDS patients should raise suspicion for malignant etiology such as lymphomas (i.e Diffuse Large B-Cell Lymphoma) and disseminated infection such as Mycobacterium Avium Complex (MAC). Disseminated MAC often involves lymph nodes, spleen, liver, or bone marrow. MAC is considered an AIDS-defining condition and is often seen when CD4 count reaches below 50 cells/µl. Disseminated MAC may lead to symptoms such as pericarditis, arthralgia, or CNS involvement in the form of brain abscess. In conclusion, this case illustrates the need for extensive diagnostic workup among AIDS patients with unusual presentations suspicious for malignancy.