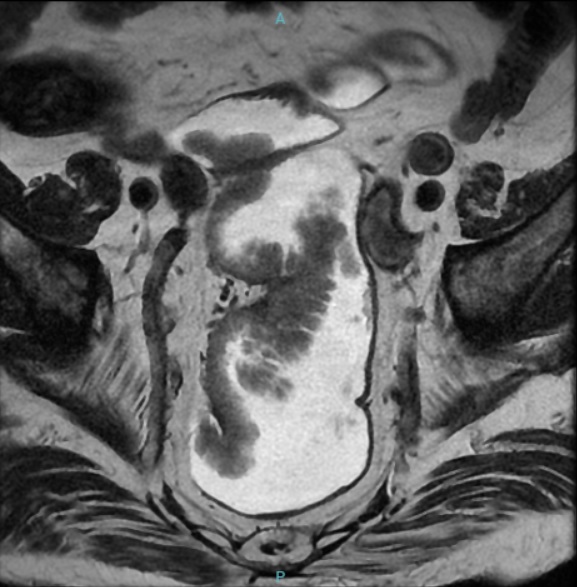
Case Presentation: A 90-year-old man with chronic kidney disease and benign prostatic hyperplasia presented with a 4-month history of persistent mucous diarrhea, abdominal pain, and a few episodes of enterorrhagia. On exam, vital signs were normal except for hypotension. He was in mild acute distress but alert and oriented. He had dry mucous membranes and extended capillary refill time. Laboratory testing revealed acute kidney injury, hyponatremia, and hypokalemia. Further evaluation with colonoscopy revealed rectal villous adenomas occupying approximately two-thirds of the circumference of the middle and lower rectum. A diagnosis of McKittrick-Wheelock syndrome (MWS) was made. Longitudinally, the lesion extended from 7 to 21 cm from the anal canal (Figure 1). After initial staging with magnetic resonance imaging and endoscopic ultrasound, no projection beyond the mucosa and no spread of metastases to nearby lymph nodes were identified (Tis N0). Due to the patient’s refusal to undergo a surgical approach, as well as frailty and high perioperative risk, we decided to consult Gastroenterology/Endoscopy to perform an endoscopic mucosectomy with a diathermy loop. The lesions were almost completely resected (Figure 2), leaving a partial central area of 15 mm that was adhered to the rectal wall, which was biopsied to exclude invasive neoplasia. Anatomopathological examination of the specimens revealed villous adenomas with high-grade dysplasia, without foci of neoplasia. The patient was discharged three days post-procedure with a cessation of diarrhea and improvement in clinical and laboratory abnormalities, sustained at follow-up outpatient visits.
Discussion: MWS is an uncommon condition in which high volumes of electrolyte-containing mucin are produced by large villous adenomas and cause chronic secretory diarrhea, volume depletion, kidney function impairment, and electrolyte disorders. While initial management consists of fluid replacement therapy, its life-threatening clinical course requires definite treatment with endoscopic or surgical resection.MWS is a rare and potentially lethal condition that demands a high clinical suspicion for adequate diagnosis and management, especially in the context of chronic mucoid diarrhea with electrolyte disturbances. Most case reports in the literature describe surgical (as opposed to endoscopic) resection of villous adenomas, via open or laparoscopic approaches. Our case underscores the importance of staging with MRI and endoscopic ultrasound for therapeutic planning. In high-risk surgical patients, a minimally invasive approach like subtotal endoscopic resection can be pivotal. This method not only aids in excluding invasive neoplasia but also reduces lesion volume and symptoms, offering a potential curative treatment when invasive neoplasia is absent.
Conclusions: The role of hospitalists in the dynamic landscape of inpatient care, especially in geriatrics, is crucial for discerning differential diagnoses and tailoring individualized therapeutic strategies. Our case highlights the importance of aligning treatment plans with elderly patients’ personal values and preferences, advocating with subspecialties for minimally invasive yet potentially curative treatments. The success of endoscopic resection in our high-risk geriatric patient with MWS due to rectal villous adenomas demonstrates this approach’s effectiveness, respecting patient autonomy and quality of life while providing a viable alternative to surgery.