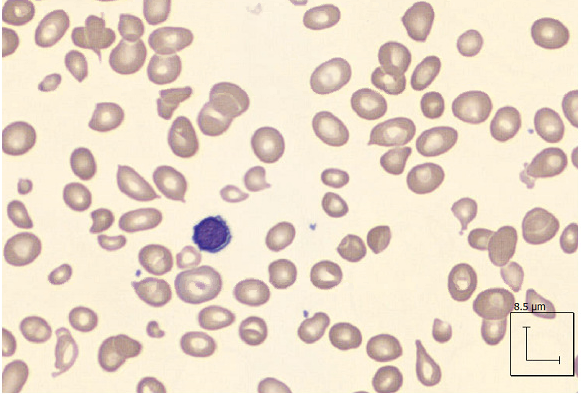
Case Presentation: Hemolytic anemia secondary to pernicious anemia is fairly uncommon, and not well described. We present a case of a 39-year-old healthy male with no significant medical history, who presented to the ED for evaluation after a near syncopal episode, along with 2 weeks history of fatigue. In the ED, vitals were unremarkable. Physical examination showed pale conjunctiva. Labs were significant for acute hemolytic anemia, as evidenced by hemoglobin of 5.6, with MCV of 109.7 fL, total bilirubin of 1.4 mg/dL, direct bilirubin of 0.3 mg/dL, LDH 2,892 IU/L, and haptoglobin <7.4 mg/dL. Thin smear showed no parasites, 2+ schistocytes, polymorphonuclear (PMN) cells with toxic granulations, and giant platelets. ADAMTS13 activity and G6PD levels were normal, tick panel was negative, direct and indirect Coombs test was negative and urine hemosiderin was negative. Further labs revealed a vitamin B12 level < 150 pg/mL, folate 14.4 ng/mL (normal), elevated Methylmalonic acid of 1.61 umol/L, positive Intrinsic Factor Ab, and Parietal Cell Ab IgG of 98.1 units. Flow cytometry was negative for Paroxysmal Nocturnal Hemoglobinuria (PNH), and no aberrant immunophenotypes were detected. Given patient’s lab values, a diagnosis of hemolytic anemia resulting from severe B12 deficiency secondary to pernicious anemia was made. The patient was then started on B12 injections, and the degree of hemolysis markedly improved throughout the hospitalization.
Discussion: Pernicious anemia is a type of megaloblastic anemia that results from a deficiency of vitamin B12, which is caused by autoantibodies to intrinsic factors and gastric parietal cells. It represents approximately 20%-50% of all causes of B12 deficiency in adults. It can present in a variety of clinical manifestations, including symptoms of anemia such as fatigue, as well as polyneuropathy and confusion. In the age group of 20 to 39, the prevalence of B12 deficiency is about 3%; and hematological abnormalities are reported in about 66% of the patients. Hemolytic anemia is a rarer presentation, presenting in only about 1.5% of patients. The pathogenesis of hemolysis is believed due to intramedullary cell death arising from arrest of precursor cells in the bone marrow, which in turn leads to elevation in LDH and decrease in haptoglobin levels. On initial presentation of our patient, the etiology was thought to be due to an acute viral infection or autoimmune hemolytic anemia, however the infectious workup, which included tick panel, hepatitis, EBV, CMV, as well as the coombs and flow cytometry were all negative. Prompt initiation of B12 replacement intramuscular 1000 mcg was done daily for one week, and repeat testing showed a decrease in hemolysis, and improvement in B12 levels. The patient was then transitioned to weekly and then monthly injections. The patient was also referred to gastroenterology for endoscopic evaluation and biopsy, as there is increased risk of gastrointestinal neoplasms. Our case highlights the recognition of pernicious anemia as a cause for hemolytic anemia, as this can have significant impact on the management of patients.
Conclusions: Pernicious anemia is one of the most common causes of vitamin B12 deficiency. Given the rare presentation of hemolytic anemia in the setting of vitamin B12 deficiency, high clinical suspicion is required to accurately diagnose and began prompt treatment. In patients presenting with evidence of hemolysis, it is important to have a broad differential of hematologic conditions, one of which includes pernicious anemia.