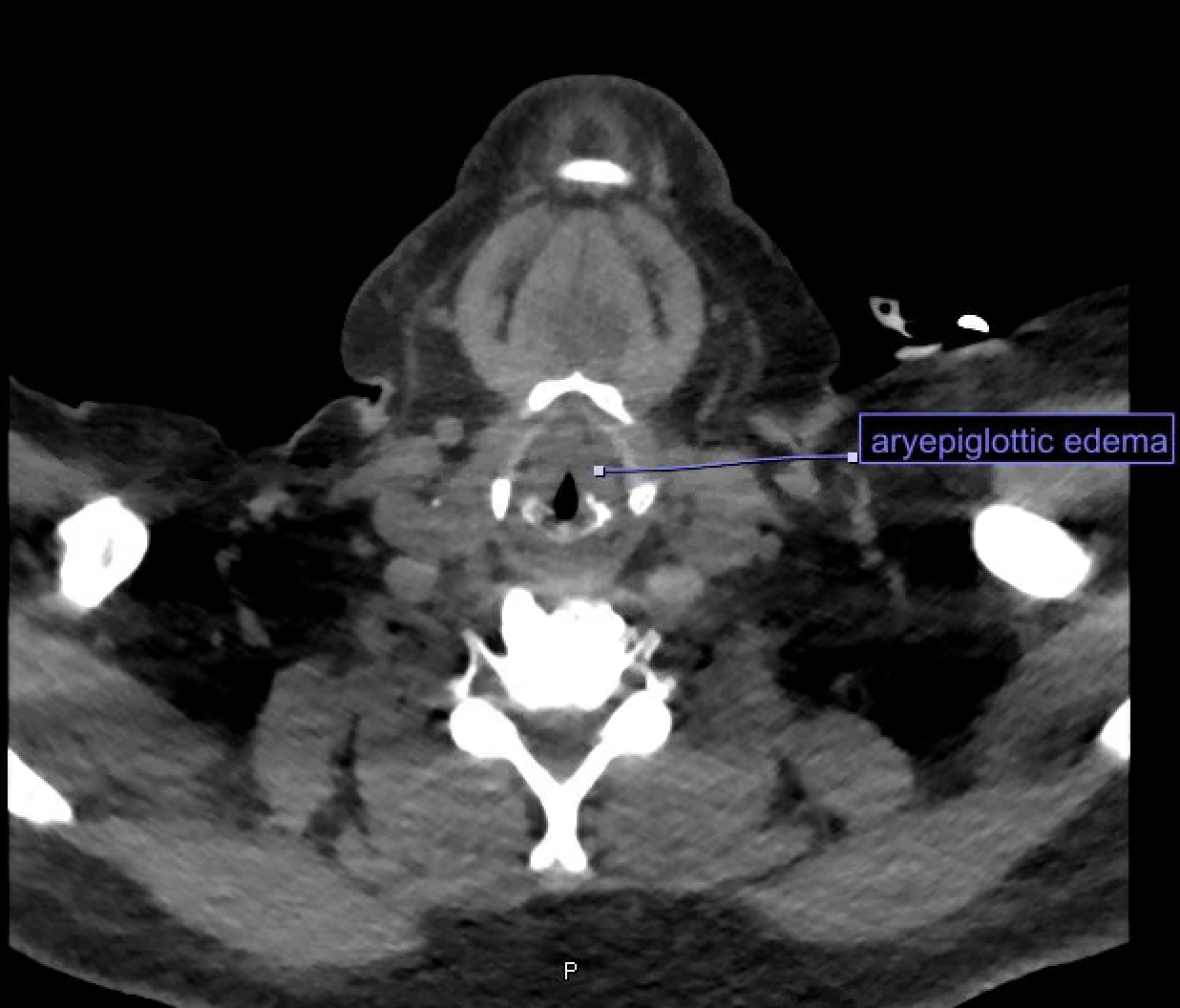
Case Presentation: A 62-year-old woman with a history of chronic kidney disease (stage 5) and acquired hypothyroidism secondary to radioactive iodine therapy for multinodular goiter presented with subacute slowed mentation, difficulty concentrating, slurred speech, visual hallucinations, and fatigue. Review of systems revealed cold intolerance, constipation, and dry skin. She was adherent to her daily levothyroxine. Exam was notable for some slowed responses, lower extremity pitting edema, xerosis, and intermittent bradycardia. Laboratory studies revealed TSH 106.399 uIU/L, Free T4 0.87 ng/dL, and stable creatinine. She was diagnosed with hypothyroidism with concern for myxedema coma (myxedema coma score 45). Endocrinology recommended IV levothyroxine and diuresis given concerns for gut edema impairing absorption of oral medications. After two days she developed a muffled voice, the sensation of something stuck in her throat, and became more somnolent. VBG revealed pH 7.29, pCO2 63 mmHg. CT head/neck showed diffuse edema throughout the superficial and deep spaces of neck, edema of the larynx and aryepiglottic folds, and airway narrowing. ENT performed flexible laryngoscopy which confirmed these findings and was consistent with myxedema affecting the vocal cords. The patient was transferred to the ICU, intubated for airway protection, treated with IV steroids, IV diuresis, IV Liothyronine, and IV Levothyroxine. Over 2 weeks her labs steadily normalized. She clinically improved and was extubated. She was discharged on an increased dose of levothyroxine and aggressive diuretic regimen with plans to start dialysis in the coming months.
Discussion: Though myxedema coma, the most severe form of hypothyroidism, is rare, its mortality rate is estimated at 30%, making early recognition essential. Myxedema coma characteristically presents as altered consciousness, hypothermia, and myxedema (swollen extremities, face, and tongue due to abnormal deposits of mucopolysaccharides). There are no universally agreed upon diagnostic criteria, though some utilize a scoring system in which a score >60 highly suggests myxedema coma and a score of 25-59 supports myxedema coma. The ‘coma’ is a misnomer and when present is usually due to respiratory depression from an impaired response to hypercapnia. Myxedema involving the larynx and vocal cords is a rare complication in myxedema coma. Otolaryngology literature demonstrates fewer than 10 reported cases of supraglottic myxedema leading to upper airway obstruction and compromise, which may be related to thyroid hormone receptors in the larynx. Supraglottic myxedema can have profound consequences especially if unrecognized, as these are technically difficult intubations. Treatment includes IV levothyroxine, aggressive airway management, glucocorticoids and often liothyronine. In our patient, attention to respiratory status and the assistance of imaging allowed for the timely recognition of supraglottic myxedema to secure her airway and transfer her to the appropriate critical care setting.
Conclusions: Myxedema in a profoundly hypothyroid state can rarely involve supraglottic structures and result in airway compromise along with a difficult to secure airway. Hospital providers should be aware of the potential for airway compromise in profoundly hypothyroid patients, monitor respiratory status closely, and consider additional evaluation for supraglottic myxedema in patients with concern for respiratory depression or airway obstruction.