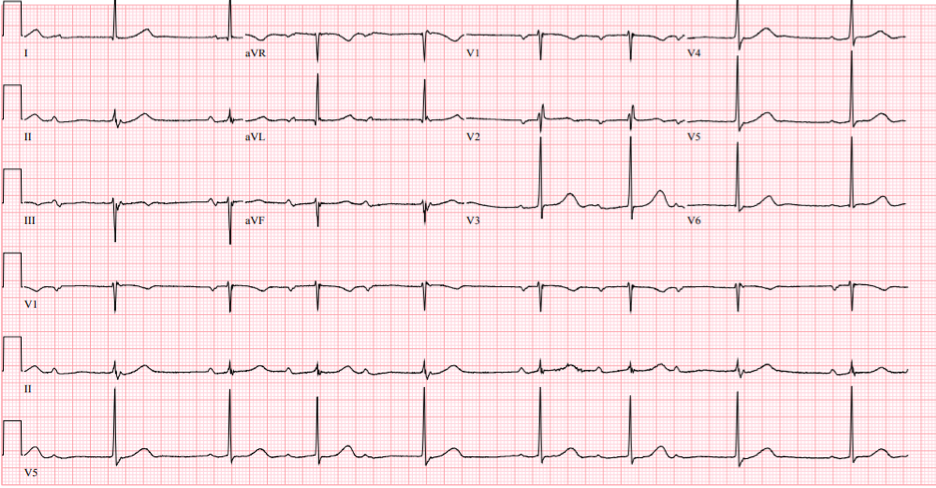
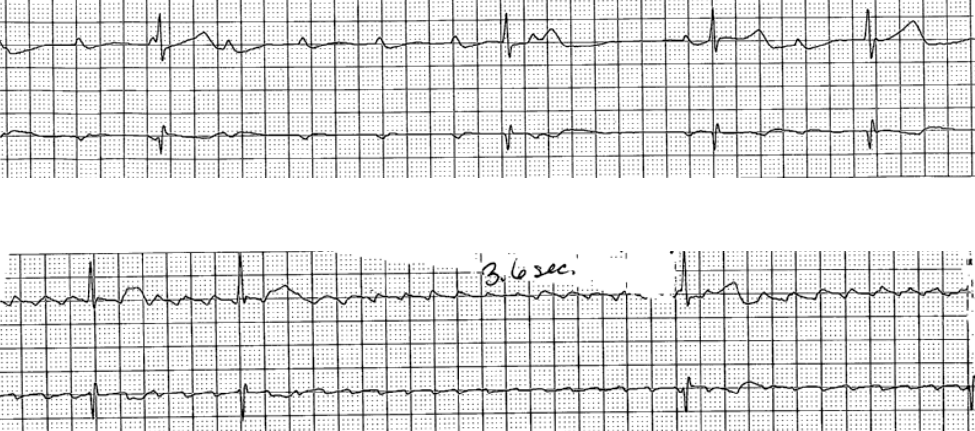
Case Presentation: An 80-year-old female with a history of type 2 diabetes mellitus presented with progressively worsening ataxia and left-sided weakness for 6 months. She had no symptoms attributable to bradycardia and was not taking AV nodal blocking medications. Examination revealed mild left hemiparesis and ataxic gait, with a heart rate of 40 beats/min but was otherwise unremarkable. EKG showed sinus rhythm with type 1 second-degree AV block with occasional SA node exit block (Figure 1). Telemetry monitoring showed transient high-degree AV block with 3 consecutive non-conducted P waves and transient atrial flutter with 3.6 seconds of pause(Figure 2). Brain MRI revealed a 4.1cm right parietal mass with prominent surrounding vasogenic edema, and 6mm leftward midline shift. Cardiology and electrophysiology recommended a temporary pacemaker prior to surgical brain mass removal. After the surgery, the patient’s rhythm was sinus bradycardia with transient, nocturnal Mobitz type 1 on telemetry without high-degree AV block or SA node exit block. The decision was made to not insert a permanent pacemaker and she was discharged.
Discussion: Multiple arrhythmias including sinus bradycardia, sinus tachycardia, wandering atrial pacemaker, paroxysmal atrial tachycardia, atrial and ventricular premature beats, various AV blocks and sinus arrest have been reported as a consequence from increased intracranial pressure. In a review article of 80 patients with cardiac alterations in the setting of an increased intracranial hypertension due to spontaneous subarachnoid hemorrhage (SAH), conduction abnormality occurred in 20% of cases, including complete heart block (7.5%), sinus arrest (4%) and type 1 second-degree AV block (4%). Reinforcing this finding, across several prospective and retrospective clinical studies, involving patients with SAH, commonly reported arrhythmias were sinus bradycardia (15%), sinus tachycardia (13%), premature ventricular beats (13%), atrial fibrillation and ventricular tachycardia (2%), AV block (1.5%), and asystole (1%). Arrhythmias due to increased intracranial pressure secondary to a brain mass may be a consequence of the Cushing’s reflex or due to a compression of important autonomic structures.
Conclusions: To the best of our knowledge, prior to this, there is no published literature that has established a causal link showing increased intracranial pressure secondary to a brain mass resulting in high degree AV block with a superimposed SA node exit block. This must be differentiated from true high-degree AV block secondary to an irreversibly damaged His-Purkinje system which requires a permanent pacemaker. In our case, a simultaneous suppression of SA and AV nodal conduction highly suggests an extrinsic mechanism of the block from increased parasympathetic tone rather than intrinsic conduction disease.