Case Presentation: Twenty-two-year-old female with history of asthma presented to Emergency Department with recurrent fevers (101-103F) and tachycardia since June 13, 2023. Patient saw her PCP on 6/10, for fever, tachycardia and abdominal pain and started on Cefdinir for possible sinusitis which she started taking yesterday. Patient had associated non-specific diffused abdominal pain, back pain, nausea, mild paranasal pain. She did not have runny nose or cough, no shortness of breath, no chest pain, no diarrhea, no urinary symptoms, no rash, no join pain or edema. No recent travel or outdoor activities, no sick contacts, no sexual activity for > 1 year. Patient has a dog, no other pets.
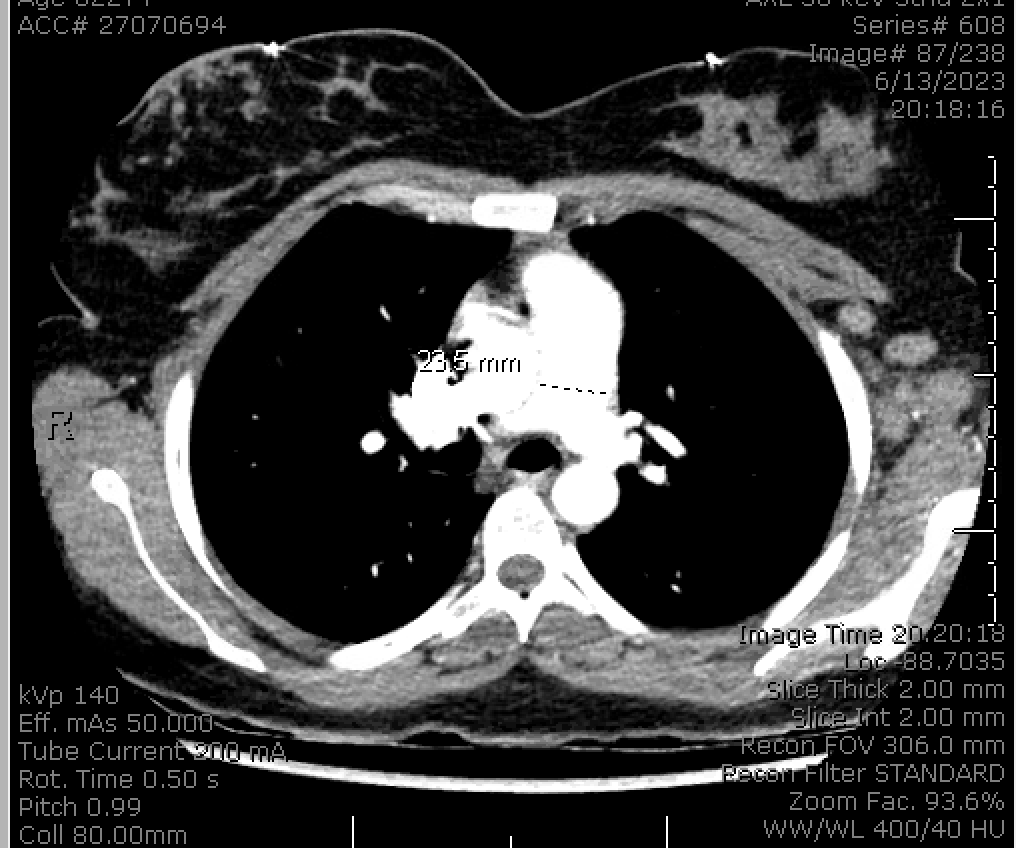
Discussion: Patient remains febrile most of her hospitalization. Physical examination was remarkable for fever, tachycardia and axillary for lymphadenopathy. Infectious work-up include RVP (negative), Group A strep PCR (negative), UA not c/f UTI, HIV ab (negative), 6/13, serial blood cultures (negative), EBV PCR (negative), CMV PCR (negative), EBV capsid IgG (positive), HIV VL (undetectable), Ticks panel (negative), ASO and DNAse titer (normal), Urine chlamydia/gonorrhea (negative), adenovirus PCR (negative), Quant-Gold (negative), toxoplasma IgG (negative), quant immunoglobulins (normal), lymphocyte subset 2 (normal).Lumbar puncture: lymphocyte 93% with opening pressure of 32, cytology (negative for malignancy), CSF culture and stain (no growth), fungal culture (negative), ME panel (negative), CSF cryptococcal antigen (negative), Bartonella (negative), parvovirus (negative).CTA PE on 6/14/23 showed bilateral increased, enlarged axillary lymph nodes that are nonspecific and may be reactive. CT AP on 6/13/23 showed no peripancreatic inflammatory changes to suggest imaging findings of acute pancreatitis without any noted lymphadenopathy.CT max/facial with few mucosal retention cysts, MRI spine without pathologic enhancement Hematology work-up: Ferritin (elevated at 1265), GGT 164 (elevated), fasting triglycerides 137 ESR 89, CRP 41, ANA (< 1:80, negative), RF (negative), C3/C4 normal, LDH elevated at 503, SSA/SSB ab negative, dsDNA AB negative, SmAB negative, SMRNP Ab negative. RNP Ab positive.Vertebral osteomyelitis or epidural abscess were r/o by MRI. Encephalitis/meningitis (E/M) was unlikely due to the LP findings and no papiledema. Lobar pneumonias, sinusitis and intra-abdominal processes were r/o by CT scans. The suspicious for infections etiologies were unlikely due to non-productive extensive work up. HLH was considered on the differential diagnosis but ferritin was not greater than 3000, and there was no splenomegaly or bicytopenia. On 6/22, patient underwent a left axillary lymph node biopsy that show necrotizing histiocytic lymphadenitis c/w Kikuchi-Fujimoto disease. The differential diagnosis for a neutrophil poor histiocytic necrotizing lymphadenitis includes Kikuchi and Lupus lymphadenitis. Although Kikuchi lymphadenitis is favored, especially in the setting of negative dsDNA. Rheumatology recommended treated with tapering dose of prednisone and NSAIDS. Patient was discharged afebrile.
Conclusions: Kikuchi-Fujimoto disease is a rare self-limited disease that affects mostly young adults of both genders. While the clinical presentation of fever could be non-specific, it may require an extensive differential diagnosis and work up. A high level of suspicious is needed and histological sample is required for the diagnosis.