Background: Throughout medical training future hospitalists have many opportunities to observe the teaching techniques of a variety of clinical instructors to inform the development of their own teaching skills. In contrast, after starting a career as an academic hospitalist there are few chances for ongoing observation of clinical teachers to refine their practice. Peer rounding creates a forum for observation and can serve as an effective faculty development tool for hospitalists interested in strengthening their clinical teaching skills.
Purpose: We developed and piloted a peer rounding program entitled HM PROF (Hospital Medicine Peer Rounding for Observation and Feedback) in our large academic hospitalist group. The goal was to provide an opportunity for hospitalists to improve their clinical teaching by observing colleagues to identify new teaching techniques to incorporate into their own practice.
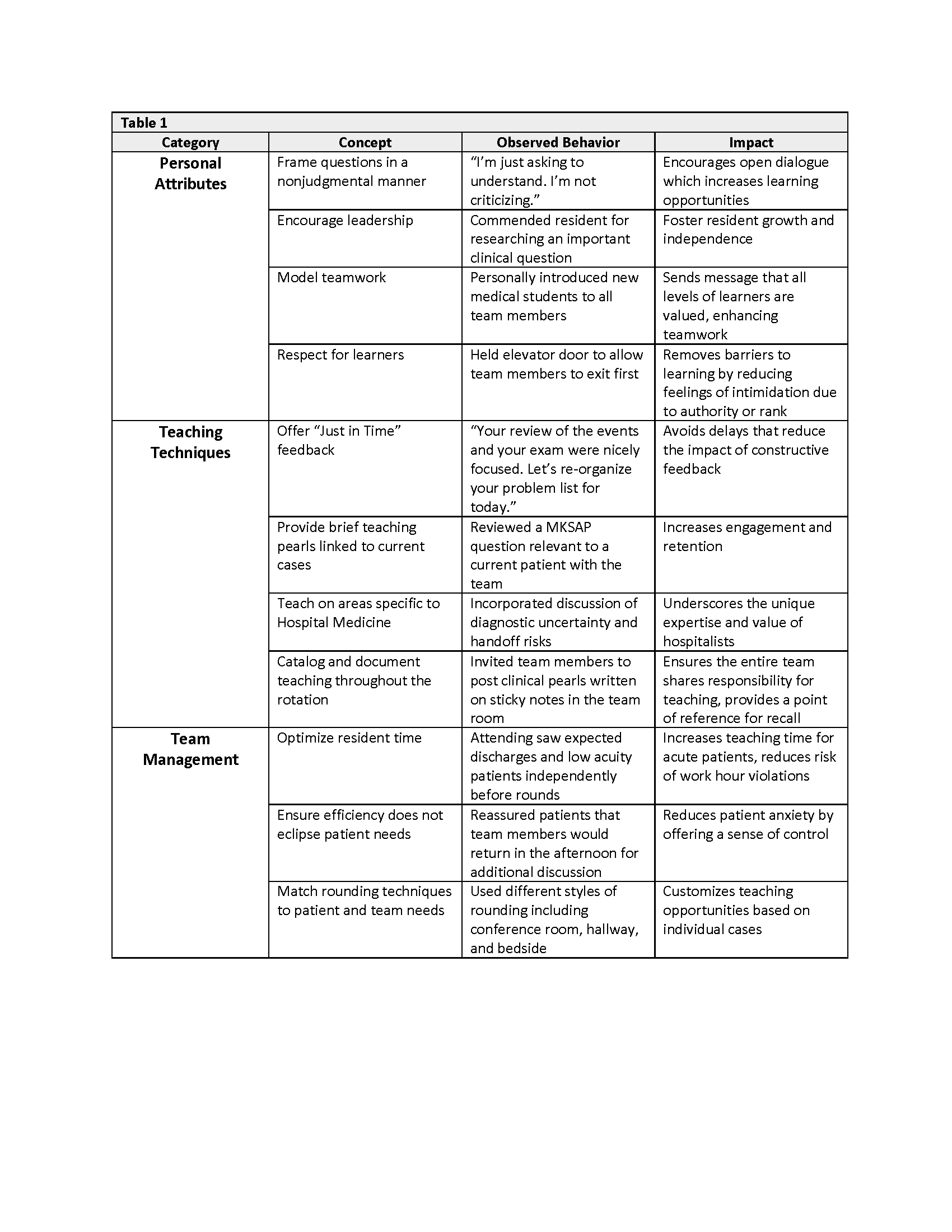
Description: HM PROF was piloted over a 6-month time period with a group of ten volunteer hospitalists. All peer rounding interactions took place during teaching rounds on the general medicine wards. Each participant was asked to, at a minimum, perform one observation and be observed by one colleague during the pilot period; due to the complexity of hospitalists’ schedules, forming observation dyads was left to the discretion of the group. Using the Stanford Faculty Development Center’s clinical teaching curriculum as a framework, we designed a document to guide observations and allow for note-taking during the peer rounding encounter. Observation dyads were encouraged to debrief in person after the observation session. Each participant was asked to complete a pre- and post-pilot survey assessing comfort of observation and peer feedback interactions with colleagues and perceived benefit of the peer rounding exercise. While the post-pilot survey results were overall positive, the small sample size precluded us from drawing any firm conclusions. Survey responses did include feedback that was used to refine aspects of the peer rounding activity, including a revision of the structured document used during observation encounters.The most valuable part of the pilot was the large number of teaching best practices recorded by hospitalists as they observed colleagues. We reviewed the de-identified observation documents and identified 27 unique “teaching pearls” which fell into three main categories: personal attributes of the attending hospitalist, clinical teaching techniques, and team management strategies (Table 1). Select pearls were shared with the division at regular intervals to disseminate best practices and generate interest in the peer rounding process.
Conclusions: The HM PROF pilot demonstrated that a peer rounding program is feasible and may be a useful faculty development tool as the majority of participants reported they identified a new teaching behavior they planned to use in the future. The pilot also generated a robust collection of useful “teaching pearls” despite the participation of a limited number of hospitalists. HM PROF is now mandatory for all division faculty and we continue to collect data with a particular interest in teaching best practices. We expect the insights gained with a larger sample size will be substantial and will serve as a valuable resource to improve the clinical teaching of the division as a whole.