Background: Deployment of Electronic Medical Records (EMR) consumes significant enterprise-wide resources. Hospitals may be reluctant to introduce further changes during the same year, including patient experience improvement initiatives. Deployment efforts may stretch clinical leaders who provide oversight on patient experience efforts. Lastly, EMR is noted to be a major source of provider burnout and deployment phase is especially stressful. As such, we hypothesize that EMR deployment would adversely impact patient experience with provider and nurse communication.
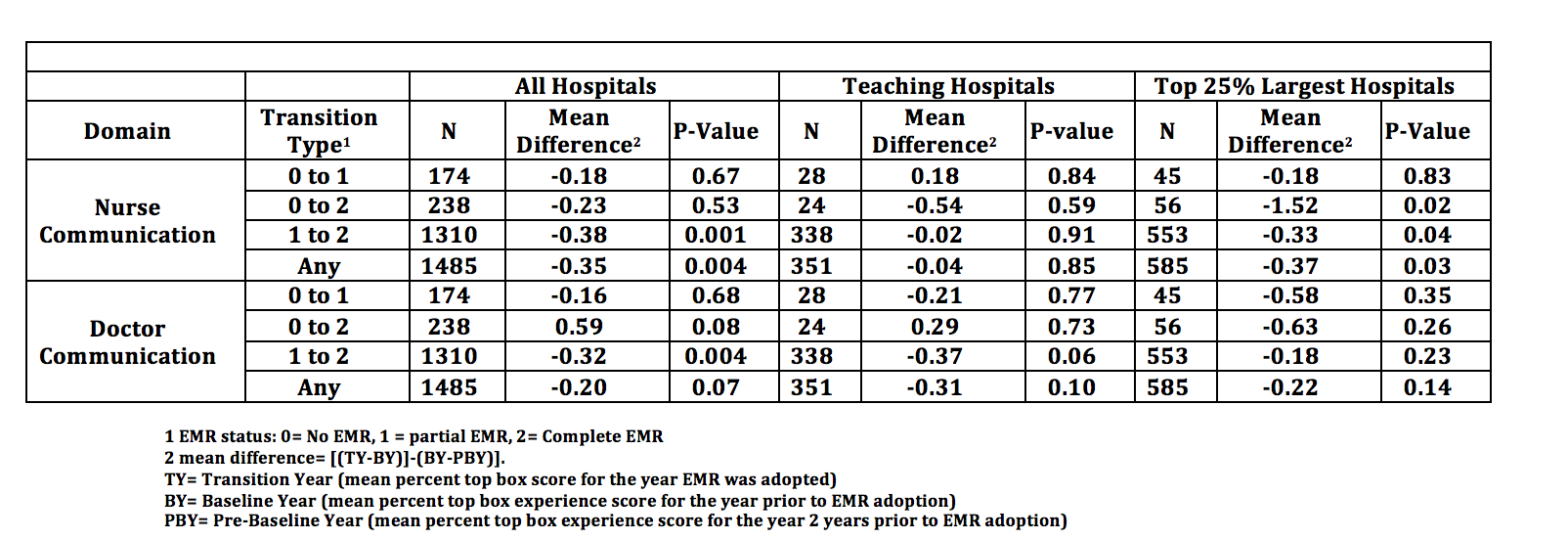
Methods: Hospital HCAHPS patient experience data were linked with 8-year American Hospital Association (AHA) data that includes hospital characteristics and EMR availability. EMR status was reported as none, partial or complete EMR. Transition year (TY) was defined as the first year when a higher level of EMR status was reported. The prior year was considered Baseline (BY) and the year prior to that was Pre-Baseline year (PBY). To account for baseline within-hospital trends, we used a difference in difference analysis using paired T-tests for provider HCAHPS scores (percent top box) between Baseline year and Pre-Baseline Year, and Transition and Baseline year [(TY-BY)]-(BY-PBY)]. Each hospital served as its own control, so we did not adjust for any hospital-level variables. Subgroup analysis was conducted for the type of transition (e.g. none to partial) and hospital type (teaching and large hospitals).
Results: There were 1485 instances reported for adoption of partial or complete EMR by hospitals. Lower nursing communication scores was associated with any type of EMR adoption (-0.35 percentage points, P=0.004) and for transition from partial to full EMR (-0.38 percentage points, P=0.001). Physician communication scores were lower for transition from partial to full EMR (-0.32, P=0.004).
Conclusions: A small but statistically significant decrease in nursing and physician communication scores was associated with EMR adoption. While the small changes may not appear clinically relevant, our assessment may underestimate the true impact. We analyzed scores for the fiscal year when the EMR adopted, whereas annualized HCAHPS scores would not capture the full impact for any EMR adoption late in the year, and because we only had access to annualized HCHAPS data, it is possible that the effects we observed resulted from more dramatic drops in patient experience of short duration. Further research is needed to assess the true impact of EMR deployment on patient experience.