Background: Inpatient physicians often discharge patients while diagnostic tests are still pending. The discharging attending is responsible for following-up these results, even if they have rotated off service. This can lead to delayed and/or missed detection of results, which impacts patient safety. It also creates a burden on physicians to check for results during time off service or even while on vacation, which can lead to physician burnout. Given the nature of shift work in hospital medicine, having a system to detect these results when physicians are off service is crucial to patient safety and hospitalist job satisfaction. The aim of our study was to decrease the time to detection of pending tests when they become available after.
Methods: A convenient sample of 10 hospitalists was chosen for our study based on the work schedule during the study period and varying experience level. We conducted a retrospective chart review of patients discharged by these hospitalists who had test results pending at time of discharge. The time to detection of results was calculated by the difference between the date and time of the test was finalized in the electronic health record (EHR), and the date and the timestamp that the result was acknowledged by a physician in the EHR. To improve performance in detecting pending results, two interventions were chosen and conducted in a staggered format. For the first intervention, the 10 physicians were given training on how best to utilize the EHR to detect pending tests. For the second intervention, the same 10 physicians were given the option of sending the pending tests to an administrative nurse, who would notify them when the test results returned so that they could act upon it. The physicians were surveyed pre- and post-intervention. Statistical analysis was performed using QI Macros.
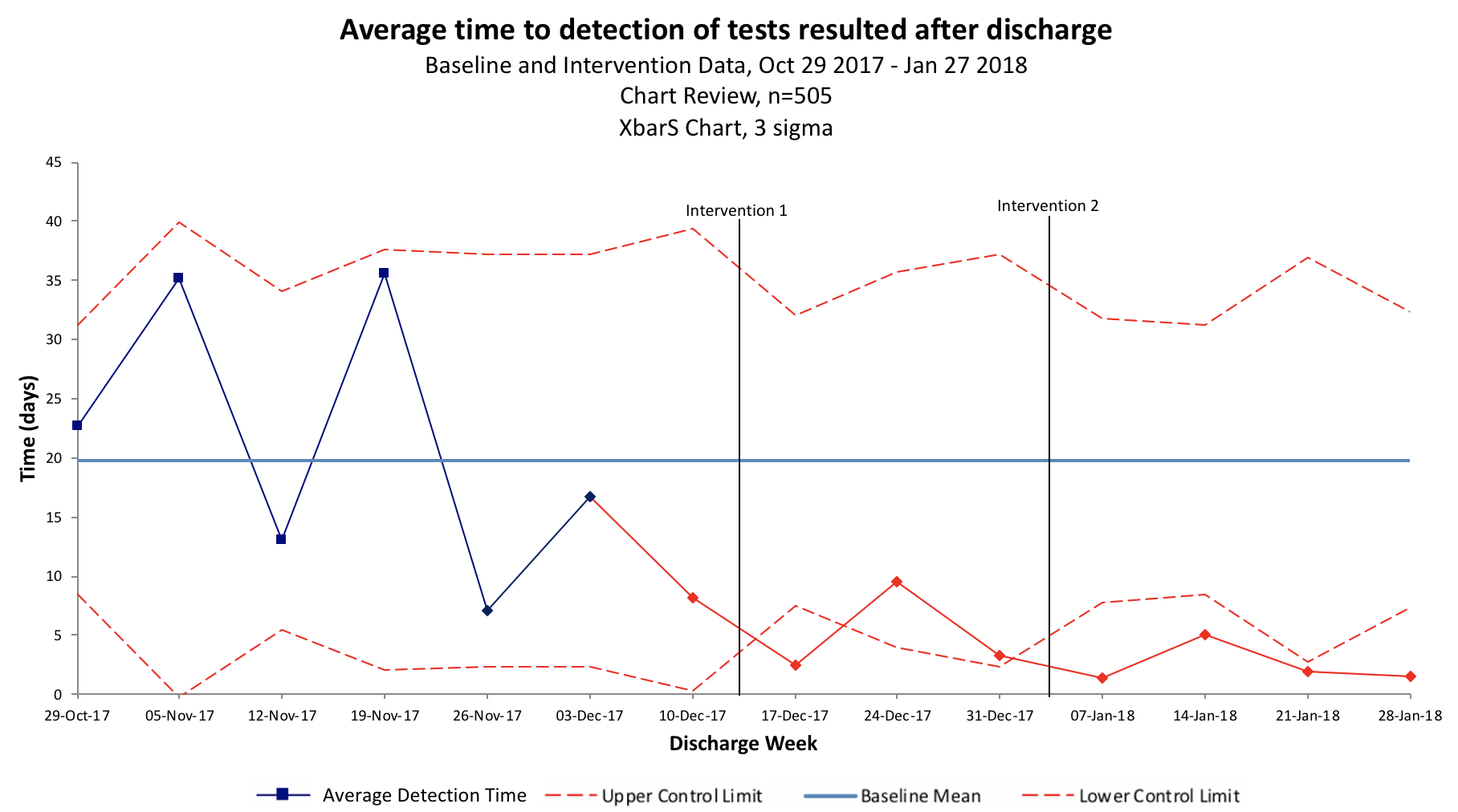
Results: From October 2017 to January 2018, 505 pending tests at discharge were identified. Pre-intervention, baseline detection time for tests that resulted after patient discharge was 19.8 days. After the first intervention, the detection time improved to 4.68 days (Figure 1). Five (50%) of the physicians completed the training, and in the survey 80% reported improved comfort utilizing the EHR, 80% reported a change in their method for detecting pending tests, and 20% reported improvement in satisfaction with their method of following pending tests. Following the second intervention, there was further improvement in detection time to 2.64 days (Figure 1). Within the second intervention period, tests sent to the administrative nurses had a shorter detection time by 1.4 days compared to those that were not. Administrative nurses reported no significant impact on their workflow. The hospitalists reported no change in satisfaction in the process of following tests using administrative nurses; nursing assistance in detecting results did not negate the necessity act upon the results even during time off.
Conclusions: Our pilot showed that EHR workflow training to manage test results after discharge improves physician comfort with the EHR and decreases detection time. The study also showed administrative assistance to track results further decreased the detection time but did not fully alleviate the administrative burden on physicians. Other means of improving detection time and burden on physicians are currently being explored by our group.