Background: The Hospital Readmissions Reduction Program (HRRP) incentivizes acute care hospitals to decrease their preventable readmissions by putting hospitals at risk of reduced Medicare reimbursements. There exist many sources of heterogeneity in the actual incentives individual hospitals face each year. The HRRP applies the same methodology to hospitals regardless of their share of Medicare patients, proportion of patients with each condition, and performance in previous years. Another potential source of incentive heterogeneity is the marginal benefit of improving readmission rates at the individual hospital level. Specifically, are hospitals that would gain the most from improving their readmission rates doing so? We evaluate whether the potential sources of incentive heterogeneity in this incentive program lead to differential performance by hospitals over time.
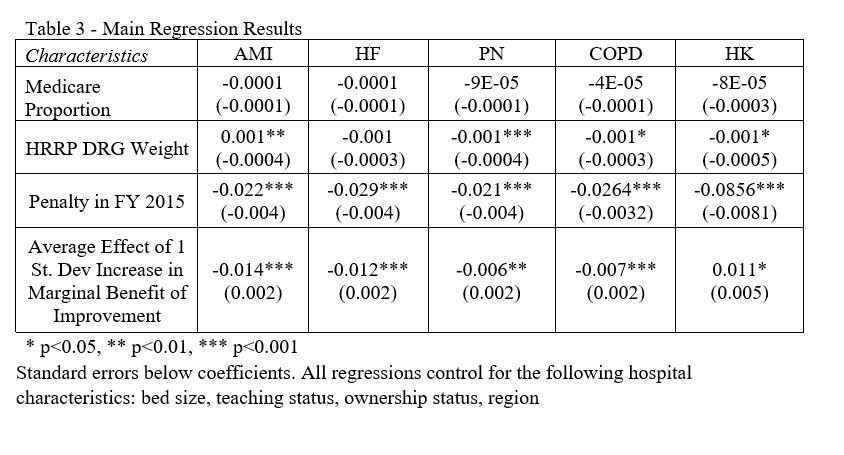
Methods: We utilize CMS Hospital Compare data from FY 2015 to FY 2018 and AHA Annual Survey data in this study. We used linear regression to identify whether various sources of incentive heterogeneity in the HRRP are correlated with changes in hospital performance over time. Specifically, we studied the effect of the following variables on changes in condition-specific, hospital-level excess readmission ratios over multiple fiscal years: proportion of hospitalized patients that have Medicare, the overall DRG share of program conditions, program performance in previous years, and a calculated condition-specific marginal benefit of improving performance on readmissions.
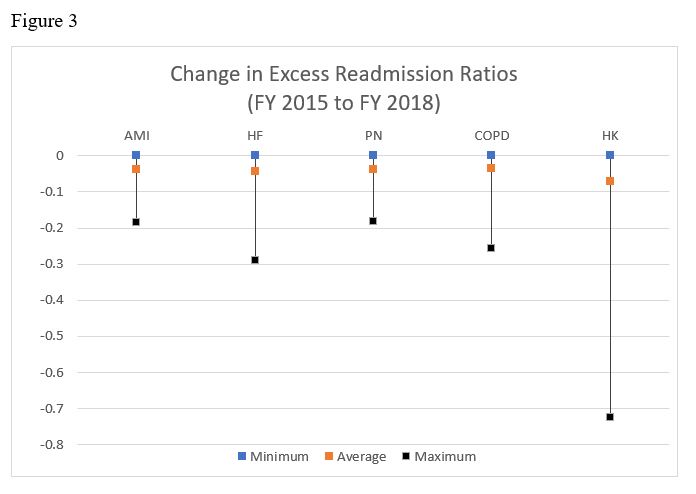
Results: We find that hospitals that received penalties in FY 2015 were more likely to improve their performance in all five conditions by FY 2018 compared to hospitals that avoided a penalty. Our regression analyses suggest that there are varying levels and directions of relationships between hospital characteristics and changes in readmission ratios over time. Our results suggest that hospitals with the most to gain in terms of their marginal benefit of improvements are doing so for acute myocardial infarction, heart failure, pneumonia, and COPD. While for hip and/or knee arthroplasty, hospitals with the most to gain from improvements may not be doing so across these fiscal years. Across all five conditions, there was no significant relationship between the proportion of Medicare patients at a hospital and changes in readmissions performance over time.
Conclusions: We find varying results when evaluating whether drivers of incentive heterogeneity for hospitals in HRRP are correlated with changes in performance over time. While hospitals did not improve to a greater degree based on their proportion of Medicare patients, we do find that hospitals are responding to the main incentive in the program; penalties levied against hospitals result in greater improvements over time in readmissions performance. In this regard, the CMS program is having its intended effect, penalties are incentivizing hospitals to work on their quality of care by reducing preventable readmissions. With our novel methodology to identify the marginal benefit of improvements on program outcomes, we find that for most conditions, hospitals do seem to be improving where there is the greatest benefit.