Background: Trauma co-management is a growing field within hospital medicine. While improvements in quality metrics have been documented in other co-management services, the impact of co-management of trauma patients is uncertain. This study aimed to determine whether a hospitalist trauma co-management program improves clinical outcomes.
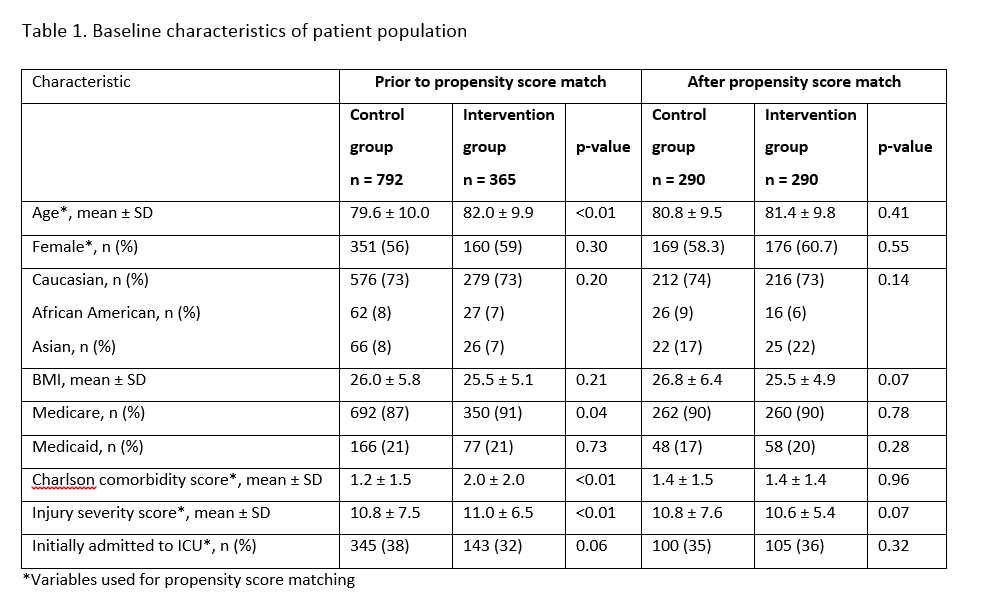
Methods: This was a pre- and post-implementation study comparing trauma surgery patients who were co-managed by a hospitalist (intervention group, January-July 2017) with patients admitted to the trauma surgery service prior to co-management (control group, January 2015-August 2016) in a level 1 regional trauma center. Criteria for the co-management service included: age > 65, history of chronic medical co-morbidities, and use of high-risk medications. The co-management service utilized the ACS TQIP Best Practice Guidelines for management of these patients. One-to-one propensity score matching (PSM) was performed based on age, gender, Injury Severity Score, comorbidity index, and initial admission to ICU. Outcomes examined were hospital mortality, length of stay (LOS), as well as quality measures (i.e. high risk medications and patterns of venous thromboembolism (VTE) prophylaxis. Differences in outcomes were compared with the Wilcoxon Rank Sum test for continuous variables and chi-square or Fisher’s exact test for categorical variables.
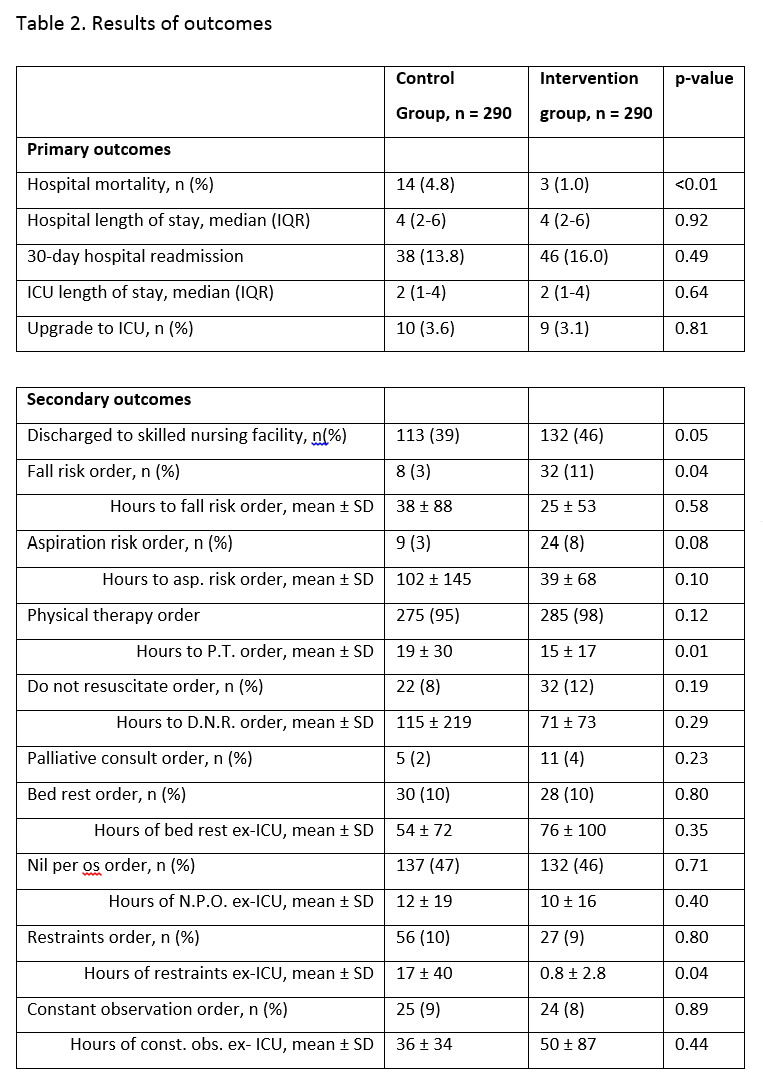
Results: From 792 control and 365 intervention patients, PSM resulted in 290 balanced control-intervention pairs. Baseline characteristics of the groups are summarized in table 1. Three patients (1.0%) died in the intervention group compared to 14 (4.8%) in the control group (p=0.0068) (Table 1). Hospital LOS, 30-day readmission, ICU LOS, upgrades to the ICU, discharge disposition were not significantly different between groups. There was an overall trend toward more patients in the intervention group having geriatrics-focused processes (e.g. fall risk, aspiration risk orders, improved management of delirium) (Table 2). Intervention patients received more doses of acetaminophen and tramadol compared to control patients (p <0.0001), and more received subcutaneous enoxaparin rather than subcutaneous heparin (p=0.0027).
Conclusions: Our study highlights that a hospitalist trauma co-management model improves quality of care without increasing LOS. Our findings add to the evidence base for the beneficial use of hospitalist co-management for trauma surgery patients.