Background: Hospitalists increasingly rely upon electronic handoff tools to communicate important patient care information. Our institution transitioned from a paper/verbal handoff process to a completely electronic system in April 2017 for day-to-night patient care handoff. In the fall of 2016, the same system had been adopted for end-of-week service change.
Purpose: This study set out to evaluate hospitalists’ utilization of an electronic handoff tool and their perceptions of its efficiency, safety and efficacy.
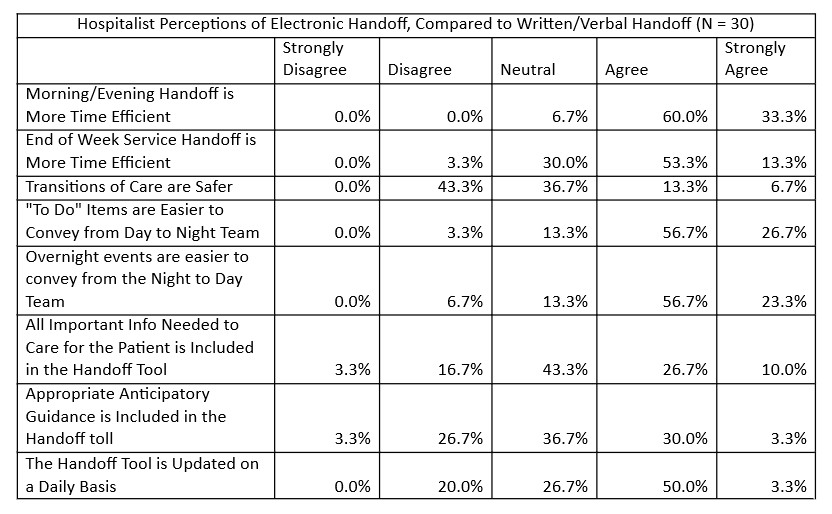
Description: We utilized the Handoff tool within the electronic health record to standardize handoffs. Day-to-night transition information is conveyed in 2 columns: “Cross-cover anticipatory guidance” and “Cross-cover To Do Items”. A similar “Service Change” list allows for end-of-week provider signout. After utilizing the electronic handoff system for at least 6 months, hospitalists were surveyed on their perceptions of electronic compared to paper/verbal handoff: see Table 1 for results
Additionally, 83% of providers stated they prefer electronic handoff to written/verbal handoff.
Tracking the utilization of the handoff tool over a 4-week period, we found that end-of-week handoff was completed 94% of the time. On an average day, the day physicians left “To Do” items for night hospitalists on 9% of patients, and night hospitalists left cross -cover notes on 22% of patients.
Conclusions: Hospitalists at our institution feel electronic handoff is (a) more time efficient, (b) easier for communicating important information from the day to the night team, and (c) preferred overall. However, 43% of providers did not agree that electronic handoff made transitions of care safer, and they had mixed opinions on whether important information and anticipatory guidance was consistently included. One provider stated that lack of in person handoff makes it more difficult to emphasize how concerned they are about a sick patient, which could potentially make patient care less safe. Another confounding factor is that around the same time we transitioned to electronic handoff, we also changed our coverage system to increase the number of handoffs that occur per day; it may be that the increased number of handoffs, rather than the electronic handoff itself, creates the perception that handoff is less safe. We are currently conveying a focus group to explore how we can make electronic handoff safer.
This study suggests that electronic handoff has strong potential to improve efficiency and communication and is well-liked overall, but Hospitalists raised concerns about safety. More study is needed to understand those concerns (including whether that large minority feel the change to safety is neutral or negative) and thus derive interventions. Analysis of safety concerns, and guidelines and standardization of information to include in handoffs may be a helpful next step.