Background: Patients with transplanted organs often have longer lengths of stay and readmissions compared to general internal medicine patients. Atypical presentations may result in unnecessary tests, missed diagnoses and incomplete treatment. Nephrologists and hospitalists bring different strengths and experiences to the management of such patients. Here we present an analysis of quality metrics as well as resident satisfaction on a transplant medicine service managed by nephrologists and the changes that resulted when this service was transitioned to care by hospitalists.
Purpose: To evaluate the impact on quality metrics when transitioning care of patients with transplanted organs from a nephrologist-based primary team to a hospitalist-based primary team over a three month period.
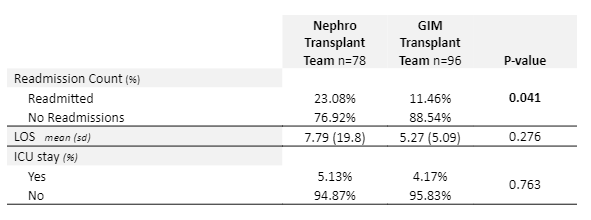
Description: The transplant medicine team at our institution cares for patients with renal transplants (greater than one year out from transplant) and lung transplants. This team was transitioned from having a nephrologist as the primary attending to having a hospitalist as primary attending with transplant nephrology on consult. A core group of eight hospitalists volunteered to serve as faculty on this service. The resident structure remained the same–one resident and one intern. We evaluated quality metrics including length of stay (7.79 days versus 5.27 days, p-value 0.276), readmissions (23.08% versus 11.46%, p-value 0.041), and ICU stays (5.13% versus 4.17%, p-value 0.763), in the three months before the transition compared to the three months after the transition. Results are presented in the attached table.
Conclusions: Transition of the transplant medicine service from a nephrology-based to a hospitalist-based team resulted in a significantly reduced readmission rate. Though there were decreases noted in the length of stay and ICU stays, the results were not statistically significant.