Background: Hospitalist models have grown significantly since their inception in the mid-1990s. However, despite their widespread presence, hospitalists’ optimal workflows remain poorly studied and defined. This gap is particularly concerning given the increasing complexity of hospitalized patients. Without a clear understanding of optimal hospitalist work design, clinicians face an increased risk of unsafe workloads and burnout, which can harm patients and providers.Time and motion studies (TMS) use observational techniques to break down activities into measurable, timed steps. When used appropriately, TMS can provide valuable insights into hospitalist workflows. However, TMS lack standardization, which limits their ability to inform evidence-based improvements in care delivery. This systematic review updates a 2010 review of TMS in hospital settings to evaluate trends in hospitalist work patterns, particularly the proportion of time spent on direct patient care, and to develop a hospitalist TMS quality assessment tool to assist with more consistent TMS design and interpretation.
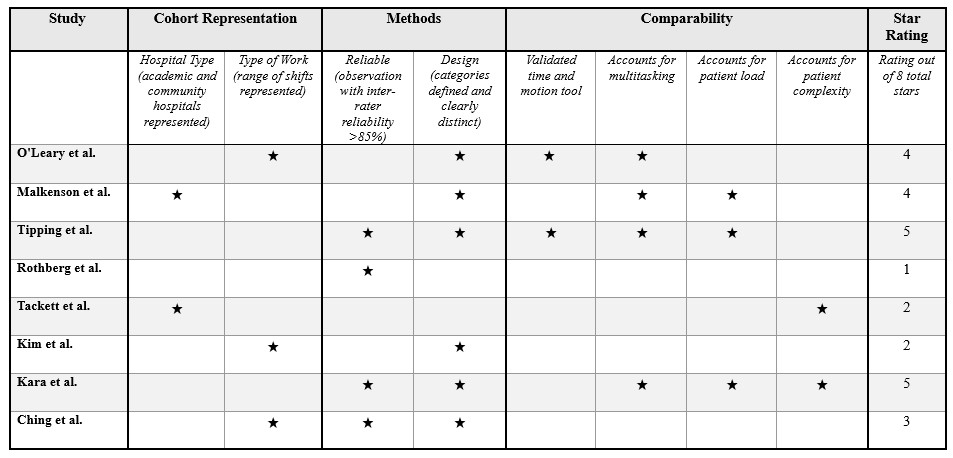
Methods: A systematic review of studies published after 1996 was performed. Databases, including Ovid MEDLINE, Embase, and Web of Science, were searched through October 2024. The authors reviewed each title and abstract to determine which merited subsequent full-text review. Studies were included if they used quantitative TMS methodologies to assess hospitalists’ time spent on direct and indirect patient care tasks in general adult inpatient care settings. Studies were excluded if they involved non-hospitalists, residents, advanced practice providers, or non-US settings. Studies were also excluded if they used non-TMS methodologies, solely analyzed activities other than patient care, or were perspective pieces, editorials, conference abstracts, or poster presentations. The authors abstracted data that focused on TMS methodologies, quality assessments, and the proportion of time spent on direct versus indirect care. A novel hospitalist TMS study quality tool was then created based on the Newcastle Ottawa quality assessment tool. Study quality was subsequently analyzed and rated using this tool.
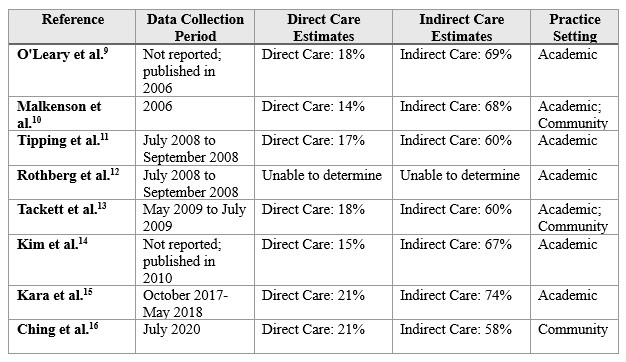
Results: Of 225 screened studies, 19 were selected for full-text review, and eight met inclusion criteria. Studies varied in cohort composition, methods, and direct and indirect care definitions (Table 1). The average proportion of time spent on direct patient care ranged from 13.8% to 20.8%. A slight increase in direct care time was observed over time, but methodological heterogeneity precluded statistical comparison. Study quality ranged from 1 to 5 stars out of 8 total possible stars, with consistent deficiencies in accounting for multitasking, patient load, and complexity. Additionally, most studies did not use validated time and motion observation tools and focused on academic hospitalists, with limited representation of community settings (Table 2).
Conclusions: This review highlights the limited nature of hospitalist TMS. Within the studies that exist, there is significant variability in TMS methodologies and quality, underscoring the need for standardized tools and approaches. Future TMS should prioritize validated methods, incorporate patient and workload-specific variables, and expand representation to include community hospitalists. As hospitalist roles evolve, reliable measurement techniques are essential to understand optimal care delivery and to improve provider well-being.