Background: For patients at increased risk of hospitalization, reducing hospitalization is often a key objective and can have important effects on health care costs. The Comprehensive Care Physician (CCP) model was developed originally at the University of Chicago to reintegrate inpatient and outpatient care under the same physician for patients at high risk of hospitalization and was found to produce large improvements in outcomes and reductions in hospitalization. While the CCP model purposively works with a group of CCP physicians and focuses on patients at increased risk of hospitalization, there are also primary care physicians (PCPs) who provide care for their patients in and out of the hospital but may not limit their practice to high-utilizing patients. We use Blue Cross Blue Shield (BCBS) Illinois claims data to identify PCPs statewide who care for their patients in and out of the hospital and compare hospitalization rates for their patients to those of patients whose PCP does not care for their patients in the hospital. We hypothesize that some PCPs continue to care to their patients in and out of the hospital, and that receipt of care from a “CCP-like” physician can decrease inpatient utilization, especially among high utilizing patients.
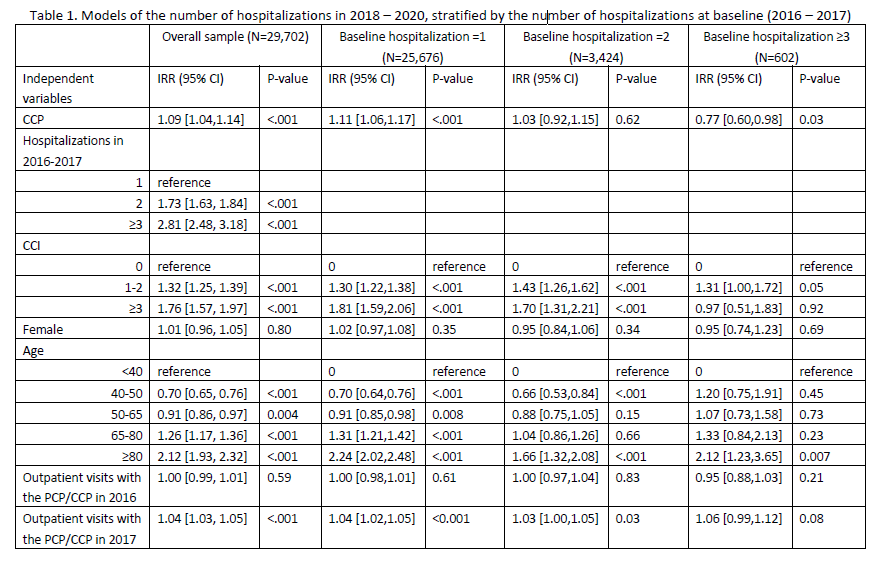
Methods: We conducted a retrospective cohort study using de-identified BCBS Illinois claims from 2016 to 2020. We identified 8,989 physicians who provided outpatient care only during the 5-year period, defined as PCPs, and 3,191 physicians who provided both outpatient and inpatient care to same patients, defined as CCPs. We identified 18,848 subjects as PCP patients and 16,668 subjects as CCP patients, among a set of patients who: (1) only visited one PCP/CCP and did not visit any other internal medicine or family medicine physician in 2016, (2) were continuously insured during 2016 – 2020, and (3) had ≥1 hospitalization in 2016 or 2017, signifying some increased patient risk of hospitalization. Propensity score matching was performed to adjust for baseline characteristics differences between CCP and PCP patients. Hospitalization rates in 2018 – 2020 were analyzed for the matched sample using negative binomial models adjusting for age, gender, Charlson Comorbidities Index, the number of inpatient and outpatient visits in 2016 – 2017.
Results: Hospitalization was significantly higher for CCP patient than for PCP patients in the overall matched sample (+9%, 95% CI 4% to 14%, p< 0.001). In subgroups stratified by the number of hospitalizations at baseline (2016 – 2017), CCP patients with 1 baseline hospitalization showed significantly higher hospitalization rate compared to PCP patients (11%, 95% CI 6% - 17%, p< 0.001). Effects on hospitalization rates were not significant for CCP vs. PCP patients with 2 baseline hospitalizations. CCP patients with ≥3 baseline hospitalizations had significantly lower hospitalization rates compared to PCP patients (-23%, 95% CI -40% to -2%, p=0.03).
Conclusions: Hospitalization rates were greater for CCP than PCP patients but reflect increased hospitalization with CCP in patients with lower baseline hospitalization rates; for patients with higher baseline hospitalization rates, hospitalization rates were lower for CCP than PCP patients. These findings suggest the value of targeting CCP models to patients at increased risk of hospitalization. Future work should assess finding generalizability by studies of larger geographic regions, examining other patient outcomes, and stratifying by risk factors such as age and health conditions.