Background: We observed improved survival among COVID-19 patients receiving remdesivir (RDV) during the early parts of the pandemic (Aug-Nov 2020) [1]. Clinical management of COVID-19 continues to develop over time as variants of concern (VOC) evolve. We extend the previous study to characterize outcomes for patients admitted on low-flow oxygen (LFO) and compare hospital all-cause mortality for early hospital RDV use vs. no RDV use across timeframes with different dominant VOC: pre-Delta (Dec ’20-Apr ’21), Delta (May-Nov ’21) and Omicron (Dec ’21-Apr ’22).
Methods: Adults with a primary discharge diagnosis of COVID-19 (ICD-10: U07.1) on LFO upon admission were identified from the Premier Healthcare Database. Patients treated with RDV in the first 2 days of admission vs. those not treated with RDV during the hospitalization were matched using a 1:1 preferential within-hospital propensity matching approach with replacement. Patients were also matched on admission month within VOC periods, and age groups. Patients were excluded from analysis if discharged within 3 days of RDV initiation. Time to 14- and 28-day mortality was examined through Cox Proportional Hazards models, adjusted for age, admission month, admission venue (ICU vs. general ward), and baseline treatments (anticoagulants, convalescent plasma, corticosteroids, baricitinib, tocilizumab). Baseline was considered as first two days of hospitalization.
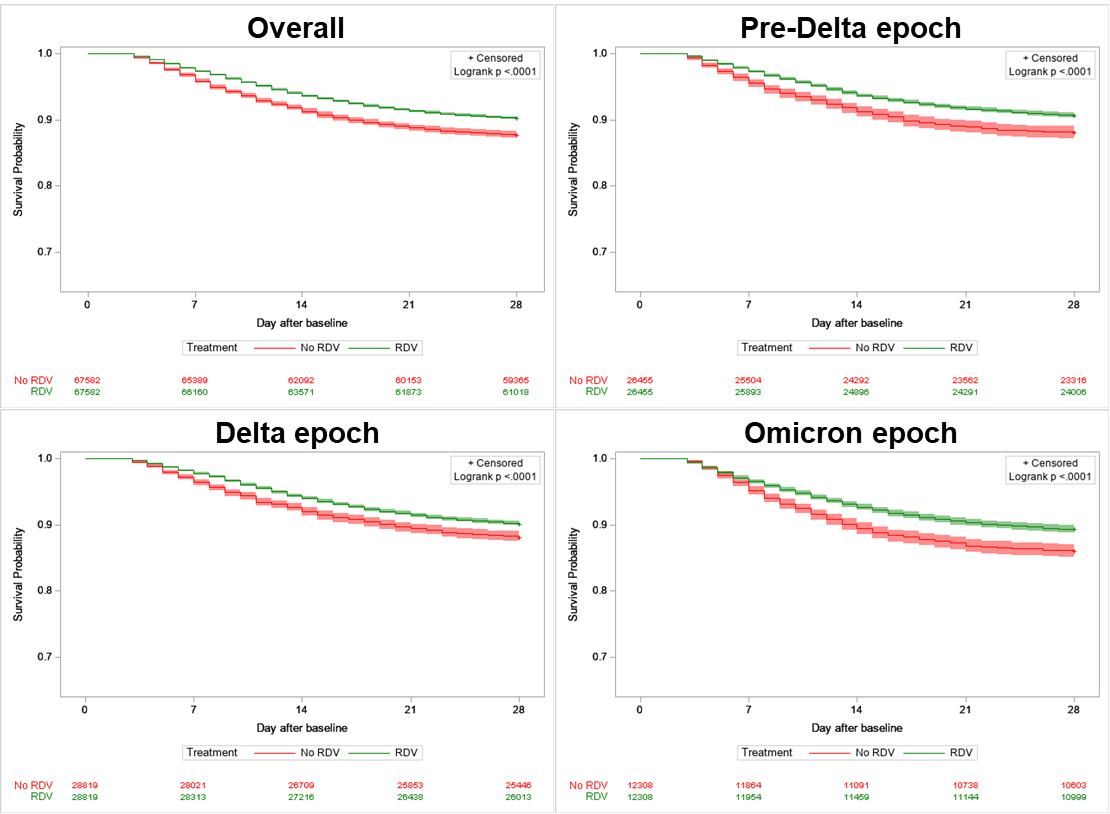
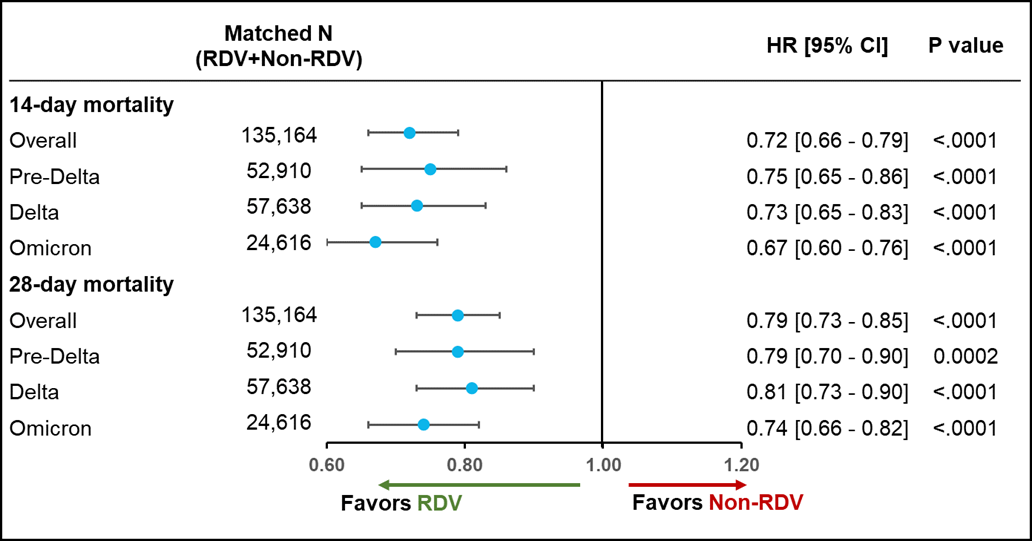
Results: Overall, 67,582 RDV-treated patients with LFO at baseline were matched to 18,830 unique non-RDV patients. The two matched groups – RDV/non-RDV were well-balanced, median age of 63 years (IQR: 52-74)/64 years (IQR: 52-74), 49%/48% female.During the overall study period (Dec 2020-Apr 2022), unadjusted mortality rate was significantly lower for RDV patients on LFO at baseline at 14 days (6.4% vs. 8.8%) and 28 days (9.8% vs. 12.3%). After adjusting, RDV patients had a significantly lower risk of 14-day (HR [95% CI]: 0.72 [0.66 – 0.79]) and 28-day mortality (0.79 [0.73 – 0.85]) compared to non-RDV patients (Fig 2).During the epoch prior to the emergence of Delta, unadjusted mortality rate remained significantly lower for RDV patients on LFO at baseline at 14 days (6.4% vs. 8.7%) and 28 days (9.4% vs. 11.9%). After adjusting, RDV patients had a significantly lower risk of 14-day (0.75 [0.65 – 0.86]) and 28-day mortality (0.79 [0.70 – 0.90]) compared to non-RDV patients (Fig 2).During the epoch in which Delta was the predominant variant, unadjusted mortality rate also remained significantly lower for RDV patients on LFO at baseline at 14 days (6.0% vs. 8.0%) and 28 days (9.9% vs. 11.4%). After adjusting, RDV patients had a significantly lower risk of 14-day (0.73 [0.65 – 0.83]) and 28-day mortality (0.81 [0.73 – 0.90]) compared to non-RDV patients (Fig 2).During the epoch correlating with the emergence of the Omicron variants, unadjusted mortality rate continued to be significantly lower for RDV patients on LFO at baseline at 14 days (7.3% vs. 10.5%) and 28 days (10.7% vs. 14.0%). After adjusting, RDV patients had a significantly lower risk of 14-day (0.67 [0.60 – 0.76]) and 28-day mortality (0.74 [0.66 – 0.82]) compared to non-RDV patients (Fig 2).
Conclusions: Timely initiation of RDV within first two days of hospital admission demonstrated significant mortality reduction (>20%) in patients requiring low-flow oxygen and hospitalized for a primary diagnosis of COVID-19. These benefits were seen across the epochs of the pandemic to-date, with benefit maintained upon the emergence of Delta and Omicron VOC periods.