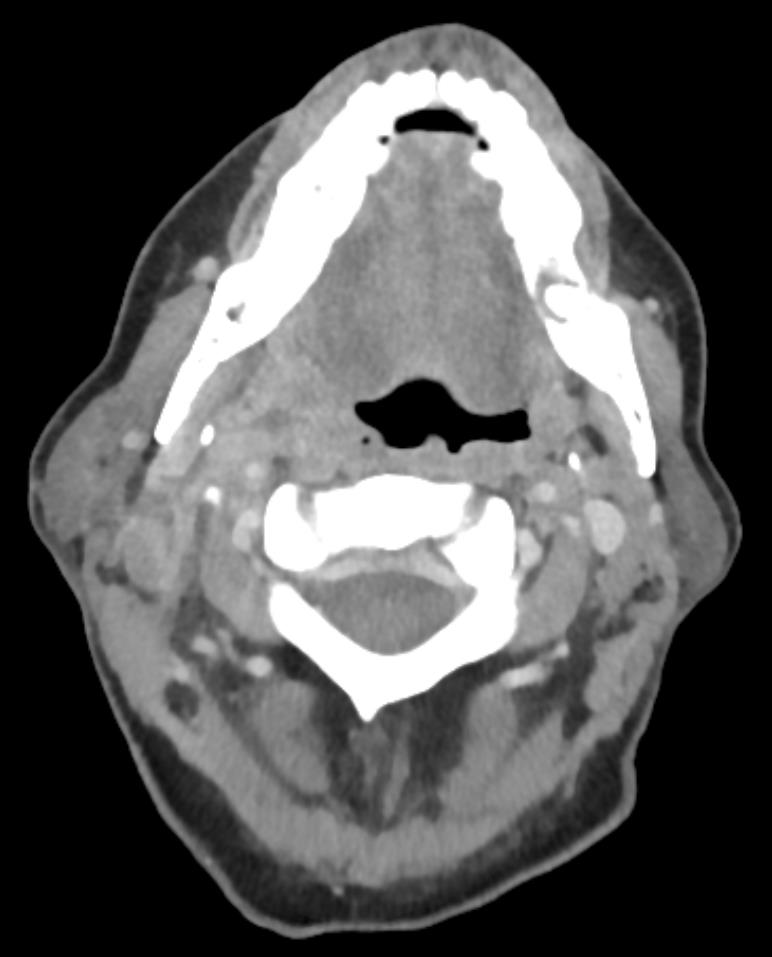
Case Presentation: A 59-year-old male with history of liver cirrhosis secondary to hepatitis C presented with right-sided jaw pain and swelling. Two weeks prior he developed a sore throat and fever. He started taking amoxicillin prescribed for him by his primary care physician and the sore throat and fever resolved. A week later he developed fever, pain and swelling in his jaw, pain with swallowing solids and liquids, and difficulty opening his mouth. Physical exam showed vital signs within normal limits, afebrile, right parotid gland enlargement and tenderness, no tenderness or swelling of the left parotid gland and submandibular glands, no lesions, erythema, or swelling in the mouth or throat, midline uvula, lungs clear to auscultation with good air movement, no lesions on the skin, and no tenderness, erythema, or swelling of the joints. Labs were notable for white blood cell count of 18×109/L with 95% segmented neutrophils and lactate of 11.4mmol/L. A CT with contrast of the head and neck showed gas bubbles, fluid collections, and swelling of the soft tissue involving the palatine tonsil, nasopharynx, and carotid space with no drainable abscess. The internal carotids and jugular veins were patent. Ampicillin-sulbactam and clindamycin were started empirically, but switched to piperacillin-tazobactam when blood cultures grew gram negative bacilli. When the organism was identified as Bacteroides fragilis, the antibiotics were changed to ceftriaxone and metronidazole. A repeat CT scan of the head and neck four days later revealed an increase in size of the fluid collection and thrombosis of the right sigmoid sinus, jugular bulb, and proximal internal jugular vein. The abscess was multiloculated and because of this percutaneous drainage would have been unsuccessful at completely draining the abscess. Surgical drainage was being considered if the patient did not improve. A CT chest was performed which showed evidence of septic pulmonary emboli. The patient’s throat pain and swelling improved, the bacteremia cleared and the patient was discharged on ceftriaxone and metronidazole to complete four weeks.
Discussion: Lemierre’s syndrome is an oropharyngeal infection complicated by septic thrombophlebitis of the jugular vein with embolization to the lungs, joints, and other organs. It is typically described in young immunocompetent patients with a mean age of 20 years old which typically begins as an oropharyngeal infection. This type of infection atypically presents in middle-aged individuals. The most common causative organism is Fusobacterium necrophorum. Other less common bacteria are Bacteroides fragilis, Peptostreptococcus, Staphylococcus aureus, Eikinella corrodens, and Pseudomonas aeruginosa. A PubMed search did not find a reported case of Lemierre’s syndrome caused by Bacteroides fragilis, as in the case of the patient described above. This diagnosis should be suspected when there is persistent pharyngeal infection despite antibiotics, which occurs because Fusobacterium is resistant to common antibiotics prescribed for oropharyngeal infections. A CT scan of the neck is essential to determine if there is a drainable abscess and thrombus in the veins. Primary treatment is antibiotics for 3 to 6 weeks and surgical drainage if there is no improvement from antibiotics. Anticoagulation use has not been studied to provide any recommendation.
Conclusions: Lemierre’s syndrome can occur as a complication of an oropharyngeal infection and Bacteroides fragilis may be the cause.