Background: Time motion studies are often conducted to describe activities of physicians caring for hospitalized patients with the goal of improving efficiency and patient safety. Prior work has mostly focused on trainees at academic medical centers. However, with the growth of hospital systems, most academic hospitals now have a similar number of patients cared for on teaching and direct care (non-teaching) services. Therefore, it is important to understand how attending and trainee workflow is similar and different to prioritize systems level interventions that impact both groups of providers.
Purpose: To determine how medicine interns and direct care hospitalists spend their time on the medicine wards and to assess for workflow enhancement opportunities at a tertiary academic medical center.
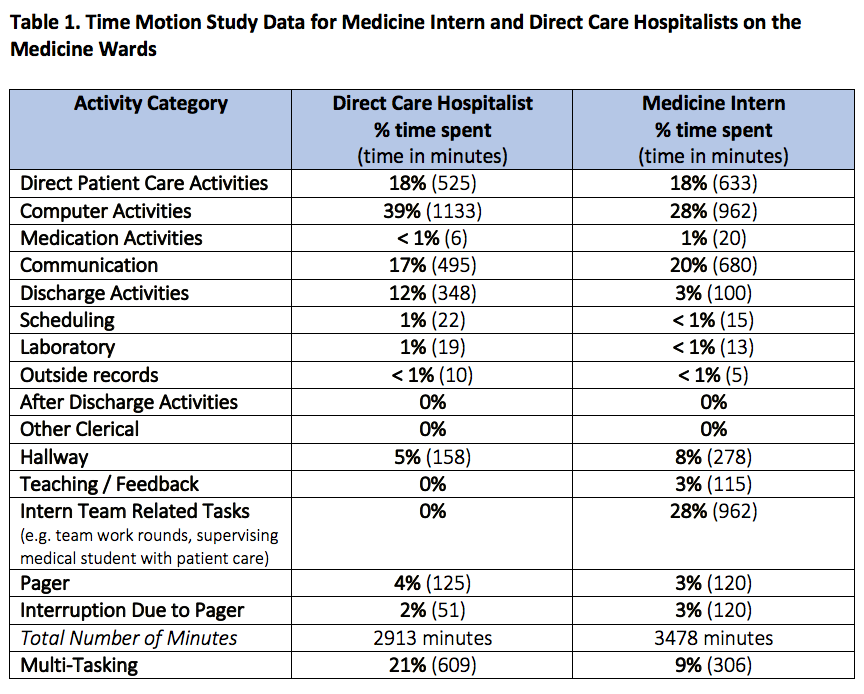
Description: Time motion studies were conducted on the direct care hospitalist and the medicine housestaff teaching service at a single site using standard data collection tools. A second-year medical student and three hospital medicine faculty performed half-day time motion studies on the direct care service, while medicine interns were observed by their peers participating in a quality improvement rotation. All observers were trained to track activities on a minute by minute basis and to record any multitasking and pager interruptions. We conducted 9 time motion studies for hospitalists (total of 2913 minutes) and 16 for interns (total of 3478 minutes).Both direct care hospitalists and interns spent the greatest amount of time on computer activities at 39% and 28% of the day, respectively (Table 1). Communication with the multidisciplinary care team consisted of 17% of a hospitalist’s day compared to 20% of an intern’s day. Direct patient care activities comprised only 18% for each individual’s day. Hospitalists spent 12% of their day on discharge activities, while interns spent 3%. Pager interruptions occurred at 2% and 3% of a hospitalist’s and intern’s day respectively. Hospitalists spent 21% of their day multi-tasking, while interns multitasked 9% of the time: most commonly chart review was combined with other tasks such as note writing, communication with consultants or order writing.
Conclusions: To our knowledge, this is one of the first time motion studies directly comparing medicine interns with direct care hospitalists at an academic medical center. Each group was similar in the amount of time spent on direct patient care, which was disappointingly low at 18% and similar to prior time motion studies in the literature. We did not identify many activities that could be easily performed by non-physician providers, although it is possible that our time study did not fully capture all of the clerical work that clinicians perform daily. However, one system level intervention that could be targeted is improved geographic localization of patients to decrease time spent walking, which equaled nearly half of the time spent on direct patient care. Direct care hospitalists spent more time than interns on computer-related and discharge activities and also spent a significantly greater time multitasking concordant activities compared to interns. This is the first study to highlight this difference in attendings verses trainees and will require further study to elucidate how this might contribute to efficiency, patient safety, and provider well-being.