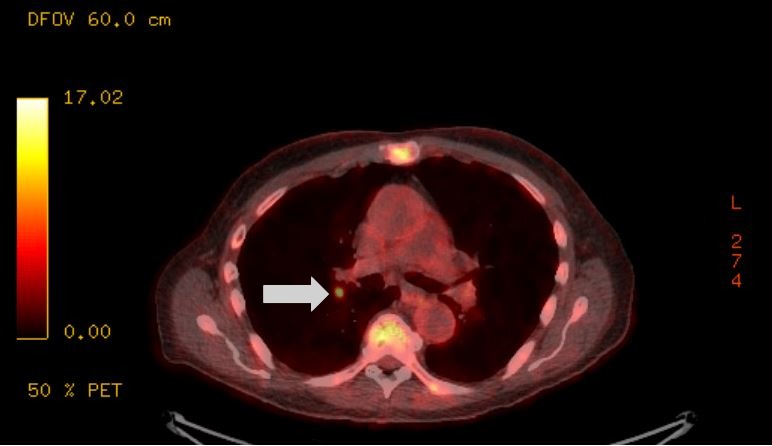
Case Presentation: An 83-year-old male with a complex medical history, including prostate cancer in remission, presented to the clinic. Routine labs revealed a serum calcium of 14 mg/dL and serum creatinine of 2.71 mg/dL and he was admitted directly from the clinic. Management included aggressive intravenous hydration, calcitonin, and a single dose of zoledronic acid. On discharge, his serum creatinine decreased to 1.9 mg/dL and calcium to 8.7 mg/dL. Notably, his prostate-specific antigen (PSA) was elevated at 9.56 ng/mL. He also had a recent history of Strongyloides stercoralis infection, treated successfully with ivermectin.Two months later, he was readmitted for recurrent hypercalcemia. Serum calcium was elevated to 14.4 mg/dL, and creatinine levels elevated to 2.37 mg/dL. Laboratory evaluation included negative infectious workups (blood cultures, serum, and urinary fungal and parasitic markers). Parathyroid hormone (PTH) was appropriately suppressed, vitamin D 25-hydroxy (25-VD) and 1,25-dihydroxy (1,25-VD) levels were within normal limits, and ionized calcium was elevated. XR skeletal survey was negative for lesions. Treatment included intravenous hydration, calcitonin, furosemide, and a dose of pamidronate.To determine the underlying etiology, the patient underwent a PET/CT which revealed subcentimeter focus of moderate FDG uptake with evidence of granulomas. Renal biopsy demonstrated non-necrotizing granulomatous inflammation. Nephrology and Pulmonary consultation confirmed a diagnosis of sarcoidosis. Given the recent Strongyloides infection, corticosteroids were initially avoided. However, the patient was later started on prednisone 20 mg daily. Following corticosteroid therapy, he did not experience further episodes of hypercalcemia.
Discussion: Hypercalcemia is a multifactorial condition, often requiring comprehensive evaluation to identify the underlying cause. The primary mechanisms include increased bone resorption, reduced renal clearance, and excessive gastrointestinal absorption of calcium. This patient’s initial presentations suggested malignancy-related hypercalcemia, given his history of prostate cancer and elevated PSA. However, diagnostic testing ruled out bone metastases, primary hyperparathyroidism, and hypervitaminosis D, prompting further investigation.Sarcoidosis-associated hypercalcemia occurs in approximately 5–10% of cases and is driven by dysregulated production of 1,25-VD by macrophages in granulomas. Diagnosis is often challenging, requiring a combination of imaging, histopathology, and exclusion of alternative etiologies; with this case requiring both renal biopsy and PET/CT.Management of hypercalcemia involves both acute treatment and addressing the underlying cause. While intravenous hydration, calcitonin, and bisphosphonates effectively lowered serum calcium levels acutely, definitive resolution occurred only after corticosteroid therapy. Steroids suppress granulomatous inflammation and reduce extrarenal production of 1,25-VD.
Conclusions: This case highlights the importance of a systematic approach to diagnosing and managing hypercalcemia, particularly in patients with complex medical histories. Sarcoidosis, while rare, should remain a consideration in cases of hypercalcemia with granulomatous findings. For hospitalists, early identification and treatment of sarcoidosis can prevent recurrent hypercalcemia and associated complications.