Case Presentation:
A 38-year-old previously healthy man presented with left flank and arm pain 72 hours after donating plasma. He noted a blister at the site of the needle insertion followed by chills. He denied intravenous drug use. Physical exam was notable for fever of 39 °C, tachycardia 113 beats per minute, blood pressure 100/65 mmHg and oxygen saturation 94% on 2 Liters nasal cannula. He was diaphoretic and his left antecubital fossa was tender, erythematous and swollen. On auscultation, he had a split S2, no murmurs and diminished lung sounds over the lung bases. The rest of his examination was unremarkable.
EKG showed sinus tachycardia and complete blood count showed White blood cell count of 14,000 with neutrophil predominance. Chest X-ray showed left sided pneumonia. Doppler ultrasound of left arm showed thrombophlebitis of the left cephalic vein. He was started on Cefepime, Vancomycin and Clindamycin. He had symptomatic improvement, however, persistent tachycardia.
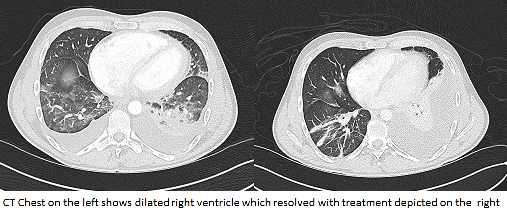
On hospital day 3, he had a fever of 38.8 °C with worsening left flank pain. EKG showed new T wave inversions in the anterior leads, troponin 0.4 μg/L. CT angiogram of the chest was negative for pulmonary embolism but revealed dilated right cardiac chambers, new moderate bilateral pleural effusions and septic emboli. Transthoracic echocardiogram showed dilated right ventricle with mild systolic dysfunction without vavulopathy. Pleural fluid analysis showed exudative fluid with normal PH and negative cultures. Blood cultures grew Streptococcus pyogenes so antibiotics were changed to penicillin G and clindamycin after which patient felt significantly improved. Follow up EKG showed resolution of T wave changes and troponins gradually trended down to 0.1 μg/L. On day 6 repeat chest CT showed normal cardiac chambers with a new 2.5 cm left lung abscess and Transesophageal echo revealed resolution of the right sided heart failure and confirmed absence of vegetation’s. He underwent ultrasound-guided left pleural pigtail catheter placement and completed 6 weeks of intravenous antibiotics with resolution of his symptoms.
Discussion:
Elevated troponins and right sided heart failure have been described in conditions other than acute coronary syndrome such as pulmonary embolism and myocarditis but this case presents transient right sided heart failure with demand ischemia in a young healthy patient as a result of septic pulmonary emboli without any evidence of valve involvement with infective endocarditis. We present confirmed echocardiographic and radiographic resolution upon tailored antibiotic coverage.
Conclusions:
Acute riight sided heart failure can occur secondary to septic pulmonary emboli which can be transient with appropriate control of the infection.