Background: Before any gastrointestinal (GI) procedures, it is recommended that patients have no intake of clear liquids (2-4 hours) and solid food (6 hours) prior to induction of sedation to minimize preoperative risks such as regurgitation, pulmonary aspiration, and other risks associated with sedation. These time frames were determined by previous randomized control trials which showed that patients had lower risks of aspiration, less thirst, less hunger, better endoscopic vision, and decreased patient discomfort when abiding by these times. However, one retrospective study found that the average nothing by mouth (NPO) time for GI procedures exceeded 12 hours, thus possibly increasing the risk of hypovolemia or hypoglycemia. Therefore, the purpose of our project was to determine the duration of NPO times and frequency of hypoglycemic events in both insulin and, non-insulin dependent diabetic patients who were kept NPO prior to an upper endoscopy (EGD), endoscopic retrograde cholangiopancreatography (ERCP), or colonoscopy procedure.
Methods: A single-center retrospective study of 42 diabetic patients over age 18 who had one of the three GI procedures between August 1st, 2023- August 1st , 2024 at Wellstar Kennestone Regional Medical Center. Patient characteristics, NPO duration times, and blood sugars levels at the time of procedures were collected via retrospective chart review. Descriptive statistics was done using chi-squared and ANOVA tests. The sample characteristics of the data were collected, and T-test and linear regression analysis were conducted to determine if prolonged NPO times were associated with hypoglycemic events.
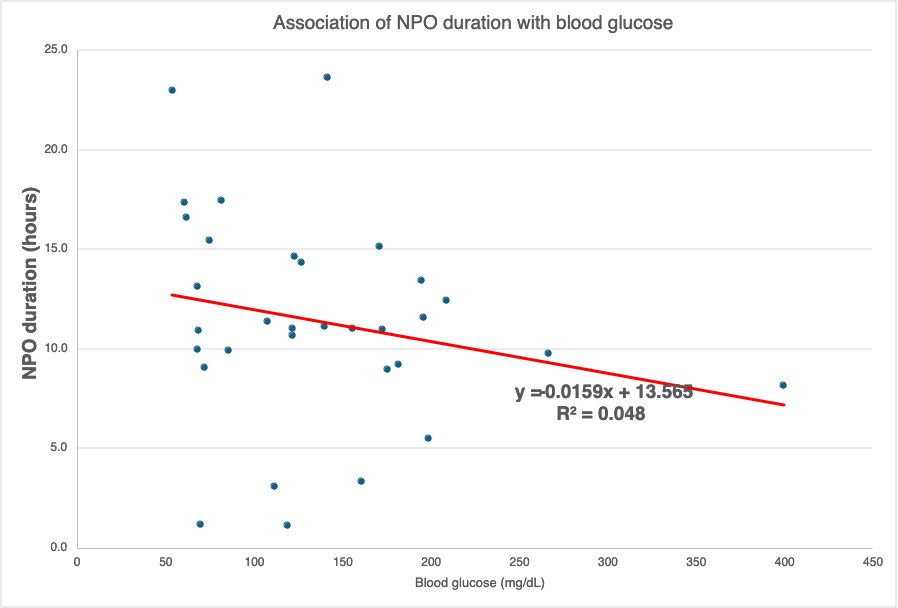
Results: Of the 42 patients included in the study, 6 had hypoglycemic events around the time of the procedure. The average age of our cohort was 64.7 years with 55% being male. The average time in hours of NPO overall was 11.31, but 15.55 +/- 1.93 in the hypoglycemic group and 10.59+/- 0.78 in the non-hypoglycemic group. Longer NPO times were significantly associated with hypoglycemic events (p=0.02). However, a linear regression analysis showed a weak relationship between blood glucose levels and length of NPO (Figure 1).
Conclusions: Our study confirmed that longer NPO times were significantly associated with hypoglycemic events in diabetic patients. Patients in our study had longer NPO times than recommended. This is important because hypoglycemia can have a high mortality. Further studies with a greater n are needed to include a multivariate regression to determine the strength of significance of our study.