Background: Inter-hospital transfer (IHT), defined as the transfer of patients between acute care facilities, is a common practice. Despite assumptions that IHT is done to provide patients with necessary specialized care, the factors which drive patient transfer are highly variable in ways that are not fully explained by differences in patients or hospitals. As such, there may be some IHT patients that are exposed to the risks of discontinuity of care without clear benefit, i.e., inappropriate transfers.
Purpose: To utilize diverse multi-stakeholder input to develop a consensus definition for potentially inappropriate inter-hospital transfers.
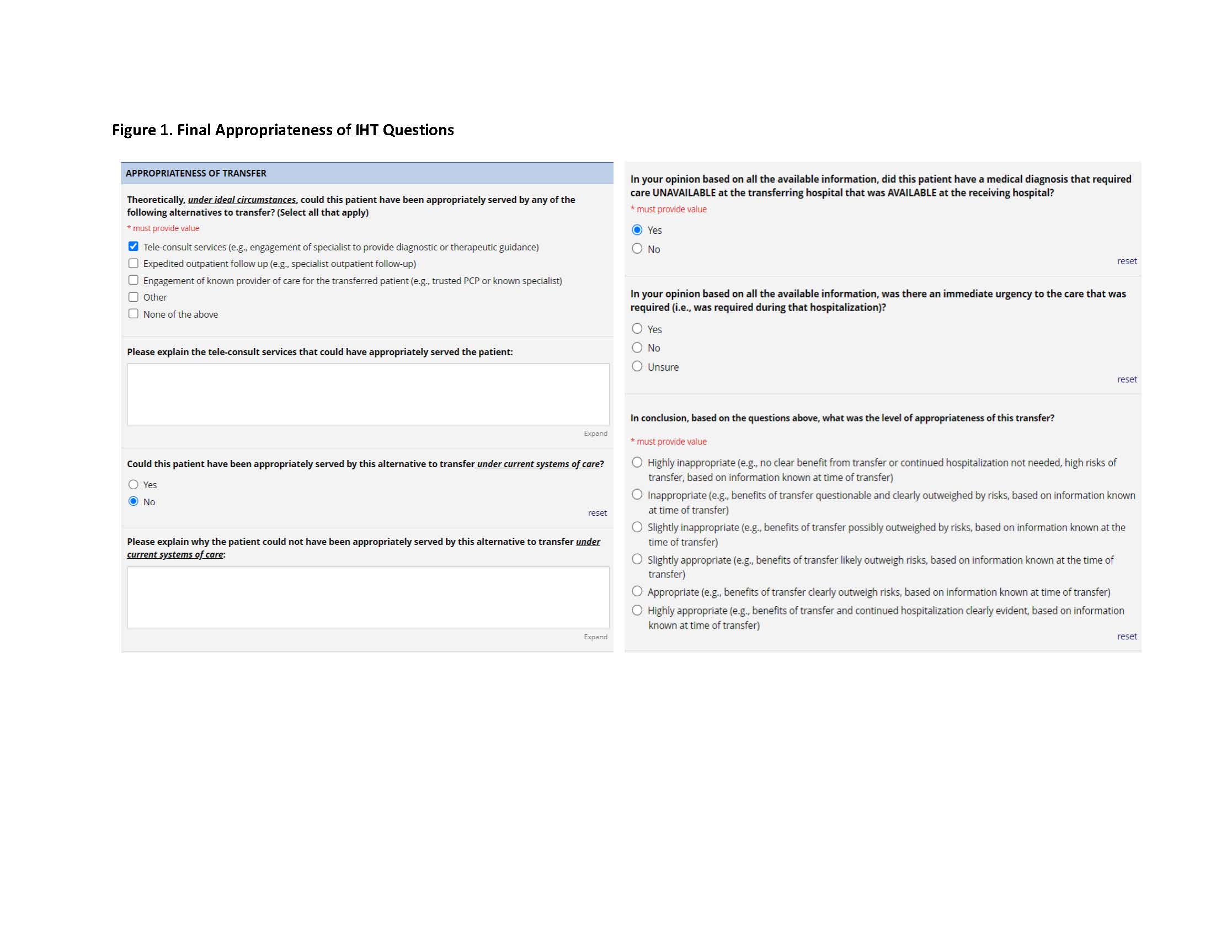
Description: During the first Aim of a 5-year study, we conducted seven 1-hour long focus groups between March and June 2023 involving 40 total participants from 13 tertiary care hospitals and affiliate referral hospitals geographically dispersed across the United States. Each focus group included 6-8 participants including at least one member from each of the following stakeholder groups: Patient and Family Advisory Council (PFAC) member; accepting clinician from a tertiary care center; transferring clinician from an affiliate referral hospital; and hospital/healthcare system leadership (Chief Operating Officer, Transfer Center Manager etc.). Discussions centered around selected IHT patient case examples and used semi-structured discussion guides to gather the perspectives of each stakeholder on the potential benefits and risks of each transfer. Discussions also incorporated consideration of environmental factors that may influence transfer (e.g., organizational/institutional relationships), potential alternatives to IHT (e.g., tele-consults), and consideration of risks of non-transfer (e.g., patient/family dissatisfaction). Sessions were recorded, transcribed and coded into major- and sub-themes by four reviewers, using a constant comparison, grounded theory approach. The final coded themes and definitions are shown in Table 1. We utilized these coded themes to modify and finalize an adjudication tool that will be used to conduct chart adjudications in the second aim of this study; this will involve targeted chart review of 1800 patient transfers to 18 geographically diverse tertiary care hospitals across the US (including the 13 hospitals involved above) to determine the prevalence of potentially inappropriate IHT. All coded themes were incorporated through the entirety of the adjudication tool. The consensus definition for potentially inappropriate IHT was incorporated within the concluding adjudication tool questions pertaining to the necessity, urgency, and appropriateness of IHT (Figure 1).
Conclusions: Based on the insight gained from diverse, geographically dispersed stakeholders in IHT, we have developed a consensus definition of potentially inappropriate IHT which has been incorporated into a finalized adjudication tool. Next steps include conducting targeted chart reviews on 1800 patient transfers across the country to determine the prevalence of inappropriate IHT and utilizing these data and ongoing stakeholder input to create best practice recommendations for the prevention of inappropriate IHT.