Background: Hospital at Home (HaH) care is an alternative to traditional hospitalization with potential to address issues of cost and hospital capacity, while improving outcomes and patient satisfaction. In 2017, the US Department of Health and Human Services began to consider bundled payments for HaH despite a lack of US-based evidence on patient outcomes, real-world participation rates, and costs. Given the potential for both patient benefits and risks, researchers should rigorously study the HaH model prior to policy changes. As part of our health system’s preliminary evaluation of HaH and who may be eligible for services, we characterized a population admitted through the Emergency Department (ED) with suspected bacterial infection and short hospital length of stay (LOS).
Methods: This retrospective study evaluated adult patients (age >=18 years) admitted to inpatient or observation status with suspected bacterial infection from January 2014 to September 2017 at 12 hospitals in the southeast. Suspected infection was defined as antibiotics ordered in the ED or within three hours of hospital admission. Because those with shorter hospital stays may be more appropriate HaH candidates, we defined two groups by LOS < 48 hours (short stay) or >= 48 hours. We then compared demographic and clinical characteristics between groups. 30-day mortality was defined by a composite of inpatient death and linked national death records. 30-day readmissions were unplanned, inpatient or observation stays at any of the system’s hospitals.
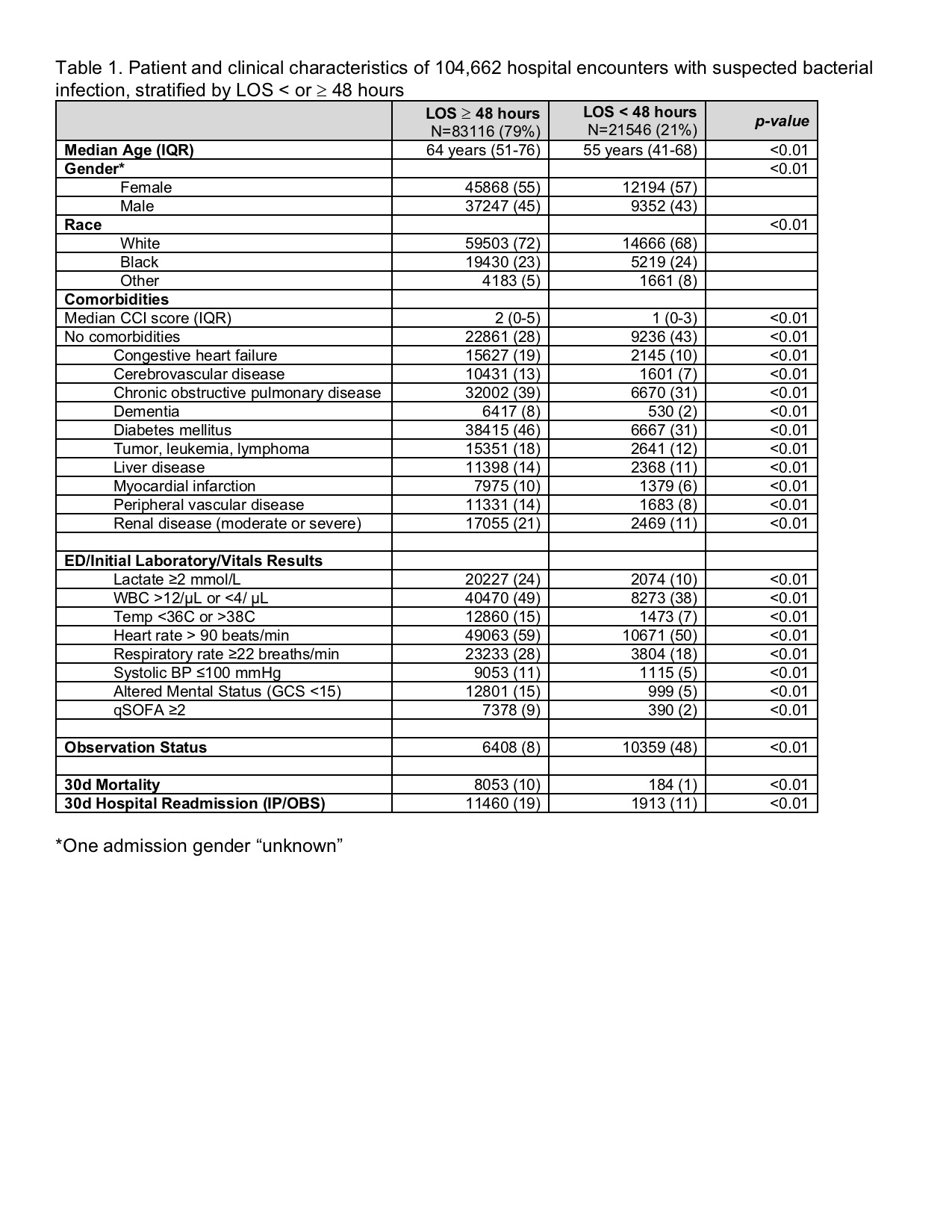
Results: 104,662 admissions met the inclusion criteria, including 21,546 (21%) short stays. All characteristics were significantly different between the two groups. (Table 1) Short stay patients were younger, had less comorbidities, and were less likely to have abnormalities in vital signs or laboratory values. The 30-day mortality and 30-day readmission rates for the short stay cohort were <1% and 11% respectively.
Conclusions: Nearly a quarter of patients admitted with suspected infection had LOS < 48 hours and comparatively better outcomes (morbidity and mortality). Additionally, in this otherwise heterogenous population, many objective variables stand out for their potential to define a large, relatively low-risk cohort that may be eligible for HaH. Next steps include development and validation of a risk model to accurately identify an acute, infected population subset at low risk for poor outcomes. After validation, this model can be deployed in a prospective, pragmatic trial of HaH, ultimately providing the critical evidence-base to inform policy decisions.