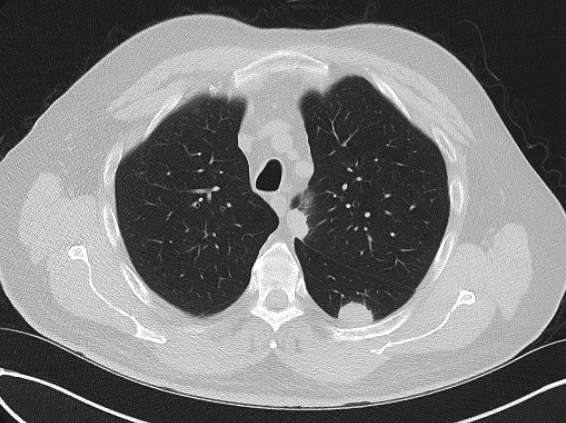
Case Presentation: Idiopathic CD4 lymphocytopenia (ICL) is a disease characterized by persistently low CD4 T-cell counts without HIV infection or any other discernible cause of T-cell suppression. Individuals with ICL are at increased risk of opportunistic infections, lymphomas, and autoimmune diseases. Diagnosis can be difficult, and prognosis can vary widely depending on the diseases that develop as a result of immunosuppression. Similarly, management is disease-dependent with no known treatment for the underlying lymphocytopenia. We present a case of ICL detected after an incidental lung nodule was found to be pulmonary Cryptococcus.A 73-year-old Guatemalan male with a history of coronary artery disease and subacute headaches undergoing evaluation for sinusitis, was seen multiple times with complaints of right-sided neck and back pain, sinus pressure, fevers, and a productive cough. He was incidentally noted to have a 9 mm left lower lobe nodule on chest radiograph, confirmed on chest CT which also showed multiple left-sided pulmonary nodules with surrounding ground glass opacities. The nodules were new since his last CT 4 months prior. Given his age, symptoms, and imaging findings, initial differential included malignancy, autoimmune processes, and atypical infections. Following negative serology and sputum induction, he underwent percutaneous biopsy which revealed fungal growth with granulomas and histological findings consistent with Cryptococcus species. Serum Cryptococcus antigen was positive at 1:64. HIV testing was negative, and although he had no known history of immunodeficiency, his CD4 count was decreased at 108 with a CD4:CD8 ratio of 0.35. His immunocompromised state coupled with ongoing headaches, blurry vision, and neck pain raised concern for disseminated infection with cryptococcal meningoencephalitis. He underwent a lumbar puncture demonstrating no evidence of central nervous system involvement with a normal opening pressure and negative Cryptococcus antigen in the spinal fluid. Given his persistently low CD4 count, he had an MRI brain which revealed a meningioma, but no other intracranial process. He underwent induction treatment with liposomal amphotericin B and flucytosine, followed by maintenance therapy with fluconazole. Subsequent imaging showed improvement of the pulmonary nodules. Serial CD4 levels remained stable in the low 100s, and HIV titers remained negative.
Discussion: ICL is a heterogeneous condition characterized by an absolute CD4 count less than 300 cells/mm3, with no evidence of infection with HIV, and the absence of any other immunodeficiencies or therapies that can suppress T-cells. According to a 2013 study, only 258 cases of ICL had been identified since the disease was first described in 1989. A 2017 report found that 75% of patients with ICL manifested with opportunistic infections, while 40% manifested with neoplasms, and 21% with autoimmunity. In contrast to CD4 levels in HIV, CD4 levels in ICL typically stabilize. No standard of therapy for ICL has been identified, but management generally consists of serial CD4 surveillance, malignancy screening, and prophylaxis if CD4 counts are less than 200 cells/mm3.
Conclusions: Our patient was found to have pulmonary Cryptococcus which led to the recognition of ICL. This case demonstrates the importance of diligent clinical investigation to diagnose ICL and provide appropriate management of potentially life-threatening sequela with opportunistic infections, malignancy, or autoimmune diseases.