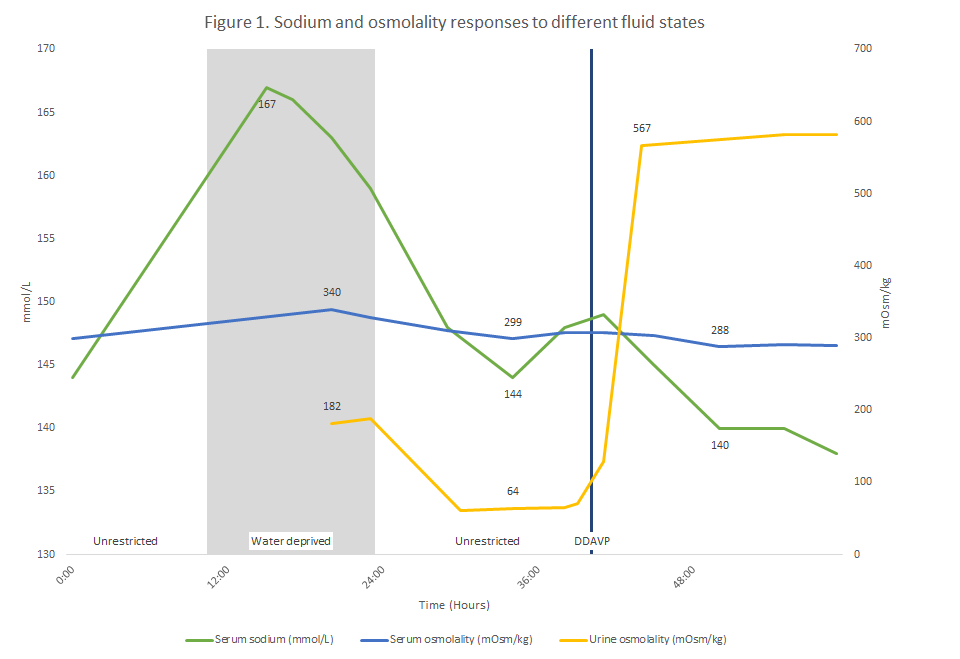
Case Presentation: A 46-year-old, previously healthy woman of Korean descent initially developed heartburn associated with thirst and frequent urination. Two months later, she presented to the Emergency Department with epigastric pain and persistent thirst. She appeared euvolemic, and her initial workup was notable for a serum sodium (SNa) of 144 mmol/L and urine specific gravity of 1.000. She received a 2 L bolus of normal saline and did not drink anything overnight. Fifteen hours later, her repeat serum Na was 167 mmol/L. Follow up testing showed concurrent serum (SOsm) and urine (UOsm) osmolalities of 299 and 182 mOsm/kg, respectively. After receiving Desmopressin (DDAVP), her UOsm increased to 567 mOsm/kg and confirmed a diagnosis of central diabetes insipidus (DI) causing hypernatremia. Her other pituitary functions were intact, and a MR Brain showed pituitary stalk thickening. No associated autoimmune, infiltrative, or neoplastic diseases were identified, and her symptoms and sodium balance stabilized on twice daily DDAVP.
Discussion: Careful evaluation of a patient’s salt and water balance helps inform the differential diagnoses for hypernatremia. This case also illustrates the importance of assessing SOsm and UOsm responses to different fluid states when evaluating polyuria. While hospitalized, patients can frequently transition between these states. In an unrestricted fluid state, patients with polyuria are able to respond to their thirst and drink enough water to compensate for urinary free water losses. As in our patient, this results in a normal or high-normal SNa and low UOsm (Figure 1). A water-deprived state eliminates this compensation and results in hyperosmolar hypernatremia. Persistently low UOsm in a water-deprived state is consistent with DI; intermediate UOsm could be due to primary polydipsia (PP) or partial DI; and high UOsm confirms PP. While hospitalized, our patient experienced an incidental water-deprived state, and her concurrent bolus of sodium likely exacerbated the resulting hypernatremia. In a third fluid state, DDAVP is administered while withholding water. A rise in UOsm ≥ 50% is consistent with central DI. Less robust responses suggest PP or partial DI, and persistently low UOsm is confirms nephrogenic DI. Many central DI cases are idiopathic, but among these, pituitary stalk thickening suggests an underlying autoimmune, neoplastic, and infiltrative condition.
Conclusions: Accurate interpretation of serum and urine osmolality must consider the underlying fluid state. In diabetes insipidus, overt hypernatremia is a very rare presentation because patients usually compensate by drinking free water.