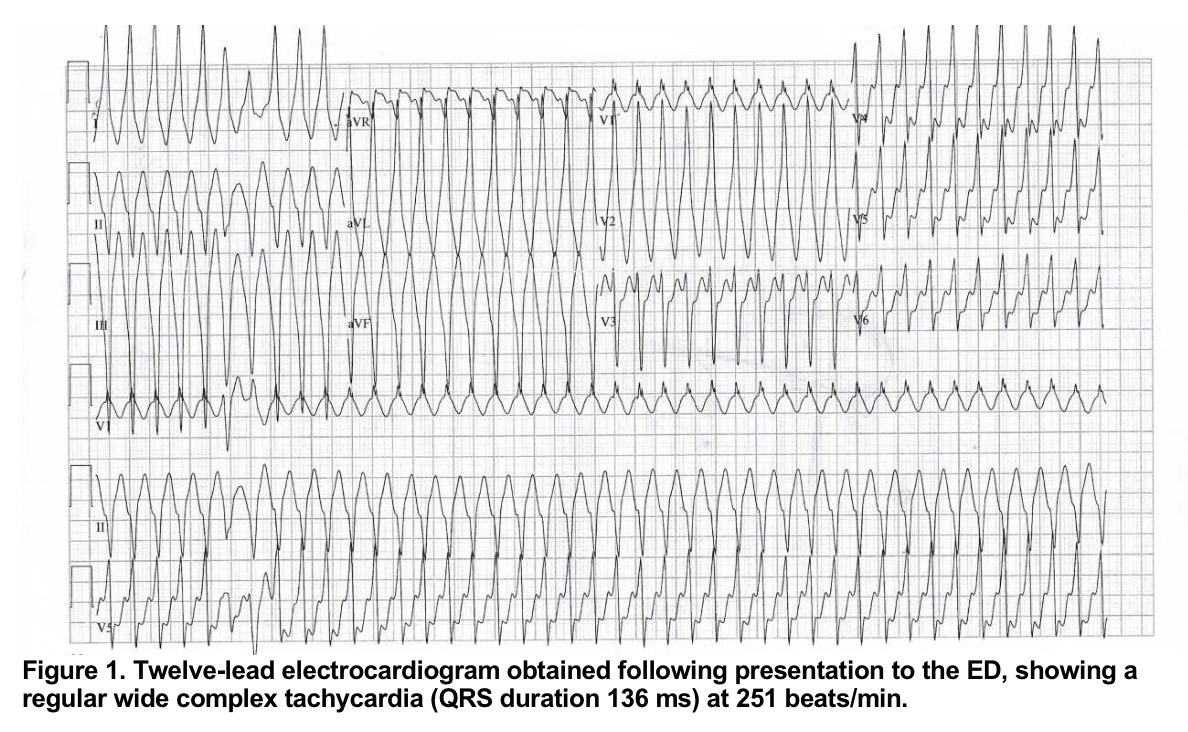
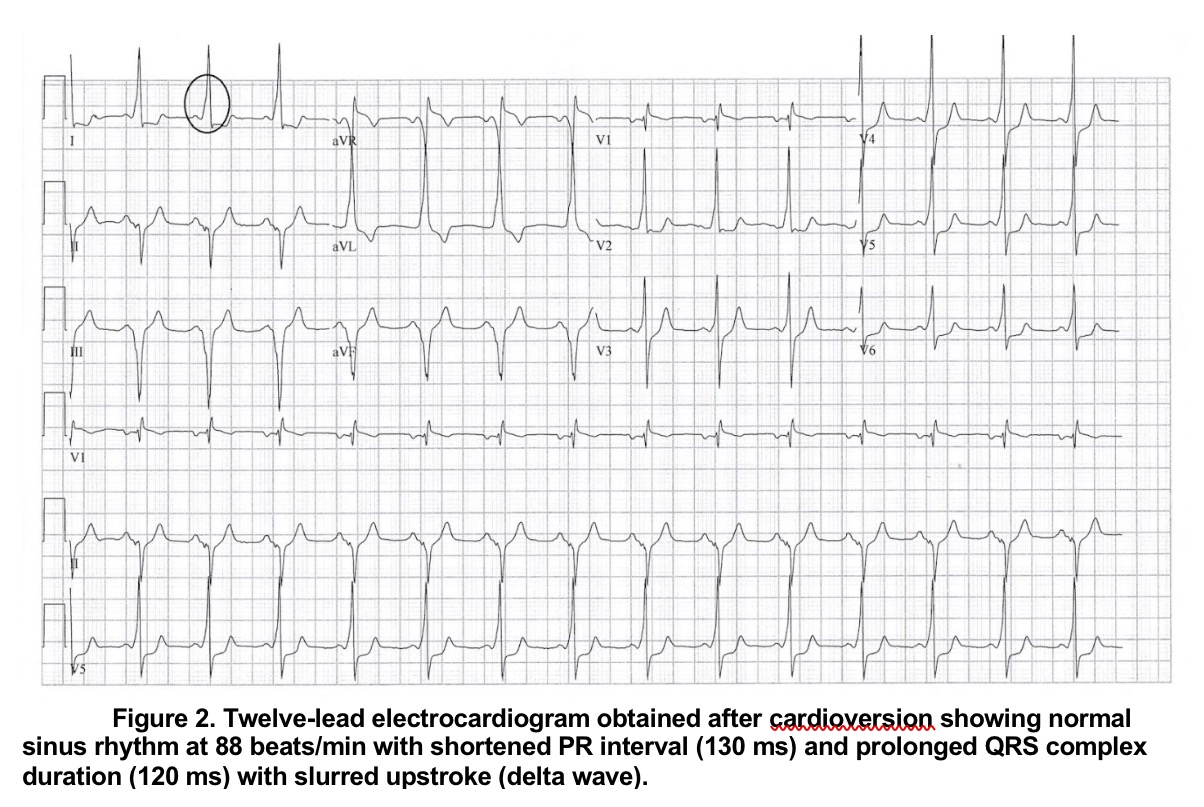
Case Presentation: A 40 year-old man presented to the hospital with a six-hour history of worsening palpitations accompanied by diaphoresis and non-radiating, retrosternal chest pain. He had been diagnosed with pre-excitation on ECG three years prior and reported a longtime history of recurrent palpitations. At the time of his diagnosis he declined any further studies. On admission, the patient’s heart rate was 251 beats/min, with a BP of 138/83 mm Hg, and his twelve-lead ECG revealed a wide complex monomorphic tachycardia (Figure 1). After determining that the patient was displaying signs of hemodynamic instability, he underwent synchronized cardioversion resulting in resolution of his symptoms. Post-cardioversion ECG showed normal sinus rhythm with classic preexcitation characteristics, including a shortened PR interval and delta waves (Figure 2). The patient later had an electrophysiology study which revealed a posteroseptal atrioventricular accessory pathway (AP), consistent with the diagnosis of Wolff-Parkinson-White (WPW) syndrome. Clockwise cavotricuspid isthmus (CTI) dependent atrial flutter (AFL) with ventricular preexcitation was induced on electrophysiology study. AFL and the AP were successfully ablated.
Discussion: We present a case of very rapid, monomorphic wide complex tachycardia (WCT) in the setting of WPW Syndrome. The typical differential of WCT includes ventricular tachycardia and supraventricular tachycardia with aberrancy. In the setting of preexcited WCT in WPW, antidromic AV reentrant tachycardia (AVRT) is typically considered. Our patient had AFL with incidental (bystander) activation of the AP, a comparatively infrequent cause of WCT. The underlying AFL was ablated, as was the AP due to its ability to sustain ventricular activation at rates that could cause hemodynamic collapse. Although the specific etiology of this patient’s tachyarrhythmia was unclear at the time of presentation, electrical conversion was required for hemodynamic instability, with resolution of symptoms.
Conclusions: In patients diagnosed with WPW syndrome who present with WCT, initial management should be dictated by the patient’s overall clinical presentation. While antidromic AVRT is more common, SVT with bystander AP conduction must also be considered in the diagnosis of preexcited tachycardia. Patients with WPW who are symptomatic or at high risk for rapid AP conduction should receive an electrophysiology study with the possibility of ablative therapy.