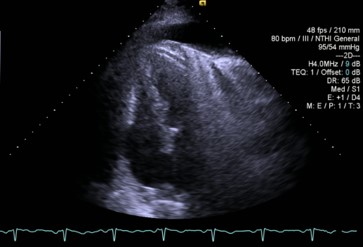
Case Presentation: A 78 year old male with a past medical history of recurrent pleural effusion and COPD who presented with dyspnea and lower extremity edema. Vitals on presentation were as follows: pulse 86 bpm, blood pressure 96/50 mmHg, 93% on room air. Physical exam revealed 2+ pitting edema in bilateral lower extremities, lungs clear to auscultation, regular rate and rhythm with normal S1 and S2. Chest X-ray on admission revealed bilateral pleural effusions. Transthoracic echocardiogram was done to evaluate for congestive heart failure showed an EF of 65%, thickened pericardium and septal bounce with reversal of hepatic vein flow. The patient’s home 4 mg PO bumetanide was converted to 4 mg IV for treatment but with limited symptom improvement. Cardiology was consulted, patient underwent left and right heart catheterization to evaluate intracardiac pressures. Catheterization revealed severely elevated right heart pressures (mRAP 18mmHg; normal RAP 2-6mmHg) and mildly elevated left heart pressures (PCWP 18mmHg; normal 4-12 mmHg) as well as equalization of diastolic pressures throughout all chambers and discordance between left and right pressure tracings consistent with constrictive physiology. Bumex was discontinued and the patient was started on colchicine 0.6mg BID for suspected constrictive pericarditis. Patient underwent pericardiectomy to treat his constrictive pericarditis. Pathology from the pericardial biopsy showed fibrosing pericarditis with positive staining for AE 1/3 and calretinin and no evidence of malignancy. He was discharged to a long term acute care after a prolonged hospital course.
Discussion: Fibrosing pericarditis is an uncommon disease state and there are not enough cases to calculate an accurate prevalence rate. This diagnosis in the absence of any clear etiology (i.e. malignancy, chronic inflammation, tuberculosis, history of radiation therapy) is quite rare and has only been described in case reports. The AE1/AE3 + staining would suggest mesothelioma, germ cell tumors, or thymoma as potential primary malignancies as the cause of the fibrosing pericardium. The calretinin positivity suggests mesothelioma as the potential primary malignancy. This case is important to note due to the exceeding rarity of fibrosing pericarditis, especially in the absence of identifiable malignancy. Therefore in patients who present with symptoms of heart failure (i.e. dyspnea and lower extremity edema) it is important to consider pericardial constriction because the prescribed therapies for these two disease entities are vastly different and each deserves proper timely care.
Conclusions: This case report aims to delve into a unique presentation of fibrosing pericarditis. These cases are very important to recognize for those practicing hospital medicine because they can appear to be straightforward heart failure but require very different management. This case surrounds a patient who presented with vague symptoms and was eventually diagnosed with pericardial fibrosis with an unknown etiology. The goal of presenting this case is to highlight a potential avenue for more research as the current literature on fibrosing pericarditis is sparse.