Case Presentation: A 69 year old man with stage IV melanoma (with brain, lung, adrenal, and gastric metastases) s/p treatment with three cycles of ipilimumab/nivolumab last 1 week ago presented with 6 days of lightheadedness, nausea, and generalized fatigue. While waiting to see oncologist bystanders witnessed the patient become unconscious with jerking motions of his right arm and leg for about one minute; the patient was unaware of this episode and could not corroborate this report. Emergency medical services were called and noted that the patient was diaphoretic and hypotensive but otherwise without complaints of confusion, incontinence, headache, cough, abdominal pain, chest pain, shortness of breath, neck pain/stiffness, pyuria/dysuria/urinary retention. Tongue biting was not observed.
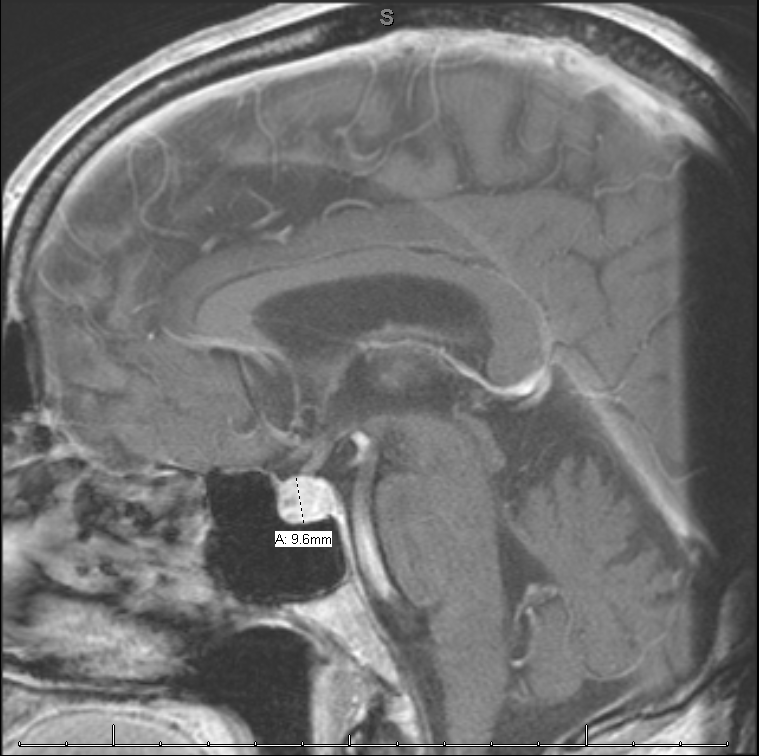
The patient was brought to the emergency department where his vital signs were notable for a fever to 100.8 and hypotension to 85/47 mmHg. He was given vancomycin, cefepime, and 2.5L NS for suspected sepsis. Laboratory analysis was notable for a white blood cell count of 10.8 thousand with a normal differential, Na 128 (mmol/L), Thyroid stimulating hormone 0.018 (mIU/L), T4 0.3 (ng/dL), cortisol 0.8 (mcg/dL), luteinizing hormone (0.3mIU/mL), adrenocorticotropic hormone (below lower limit), and urinalysis with 16 white blood cells and positive leukocyte esterase. He was started on IV hydrocortisone with a 100mg immediately followed by 50mg every 8 hours for a total of 6 doses. His hyponatremia and hypotension resolved rapidly. A brain MRI showed an enlarged and enhancing pituitary gland. CT of the abdomen and pelvis showed bilateral adrenal masses (decreased in size from priors) without adrenal hemorrhage as well as an 8mm ureteral stone. He underwent urgent cystoscopy and stone removal with stent placement. Post operatively he was started on 50mcg of levothyroxine. He was transitioned to oral hydrocortisone 50mg every 12 hours for 1 day, then 25mg every 12 hours, which is the dose that he was discharged on. He completed a total of 7 days of antibiotics 4 days of cefepime while hospitalized and 3 days of cefpodoxime.
Discussion: Hypophysitis is a well-described immune related adverse effect (IrAE) of the checkpoint inhibitors. These phenomena occur more frequently with CTLA4 antibodies such as nivolumab than with PD 1 antibodies such as ipilimumab. These phenomena can target any organ system and can occur at almost any time after administration. Most IrAEs resolve within a few months other than endocrine effects which will require long term hormone replacement. After an IrAE occurs there is debate about whether treatment regimens should be modified and if so how should they be modified. One small study found no difference in a patient’s time to treatment failure between those who did vs. those who did not modify immunologic regimens due to IrAEs. This would suggest then that modifying an immunologic regimen after a patient experiences an IrAE is safe and efficacious.
Conclusions: Consider a diagnosis of hypophysitis in any patient with previous exposure to a checkpoint inhibitor medication. The onset may be insidious and the diagnosis is often made when the condition is unmasked by some co-occuring illness such as in this case nephrolithiasis leading to sepsis and hypotension. Treatment modification may be necessary.