Background: Sleep in hospitalized adults is impaired due to several reasons. Non-pharmacological approaches should be attempted first before considering medications to treat insomnia. Environmental noise levels in the hospital are also a major culprit that might result in disturbed sleep. While limiting any disturbance or sound during sleeping hours is crucial, it might not be completely feasible in the acute care setting. Sound machine that delivers a masking noise such as white noise is reported to mask these environmental noises and promote sleep. Multiple studies have shown the sound devices to promote sleep in various settings, also they have used these in combination with other nonpharmacologic measures.1Samantha et al have reviewed the evidence regarding continuous noise as a non-pharmacological approach for improving sleep among human subjects.2We aim to analyze the efficacy and safety of sound machine on sleep efficiency in hospitalized adults.
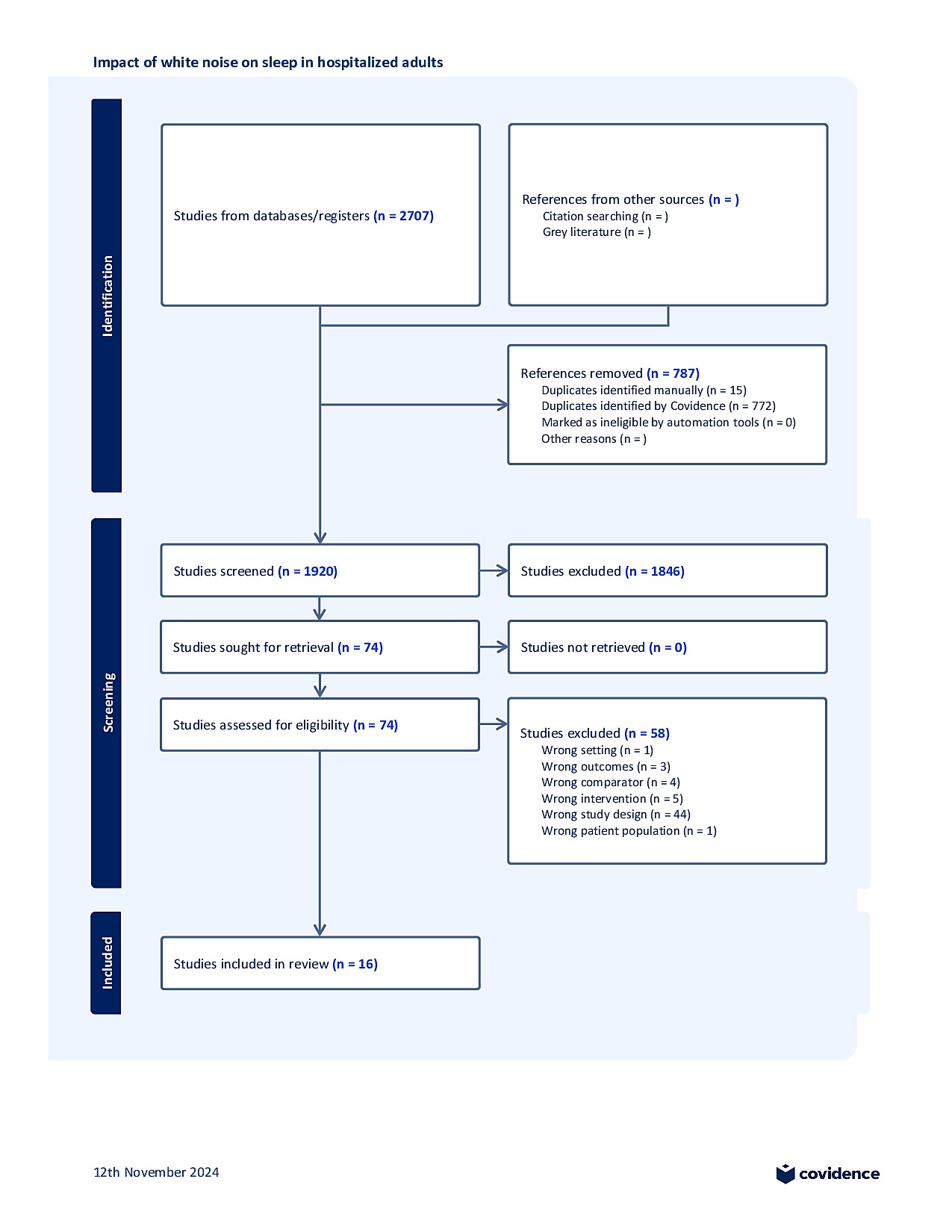
Methods: A Systematic review of all published literature was conducted following Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines. We searched MEDLINE, Embase, Cochrane database, EBSCO CINAHL, Google scholar, APA PsycINFO, Web of Science, and Scopus from inception to August 13, 2024. All studies reporting sound machine-based interventions on sleep efficiency in hospitalized adults were included. Sleep efficiency and other sleep related outcomes as total sleep time, latency, awakenings, and total sleep score were noted. Cochrane Risk of Bias 2 for RCTs was used to evaluate study quality. This study was registered with PROSPERO (CRD42024595293).
Results: A total of 1920 studies were screened, of which 74 were selected for full text review. Seven RCT studies (n = 496 participants) met the inclusion criteria and were included. Two studies were from USA, and India each, while one study was reported from Iran, China, and South Korea. Six of the seven studies used white noise, while one study reported using Uncorrelated Signal and Ambient noise in Space Integration (USASI) masking noise. Two studies report using Pittsburgh Sleep Quality Index (PSQI), and Richards Campbell Sleep Questionnaire (RCSQ) each to measure sleep outcomes. White noise was well tolerated with no major adverse effects reported, and only 8 participants discontinued the study due to discomfort or found it as low acceptability. Collectively, these studies provide evidence of improved sleep efficiency with white noise use in hospitalized adults. Given the heterogeneity in the duration of white noise use, inclusion criteria, and the outcome measurement scales in this small sample of RCT studies, meta-analysis was not feasible.
Conclusions: White- noise and other similar masking noises seem to improve sleep efficiency in hospitalized adults, with good tolerability. Only limited studies report the efficacy and demonstrate wide heterogeneity in the duration of masking noise use, varied inclusion criteria, and outcome measurement scales. Larger studies analyzing the hospitalized patient population type, across different units, to identify the best patient population who would benefit from these masking sounds are needed.