Background:
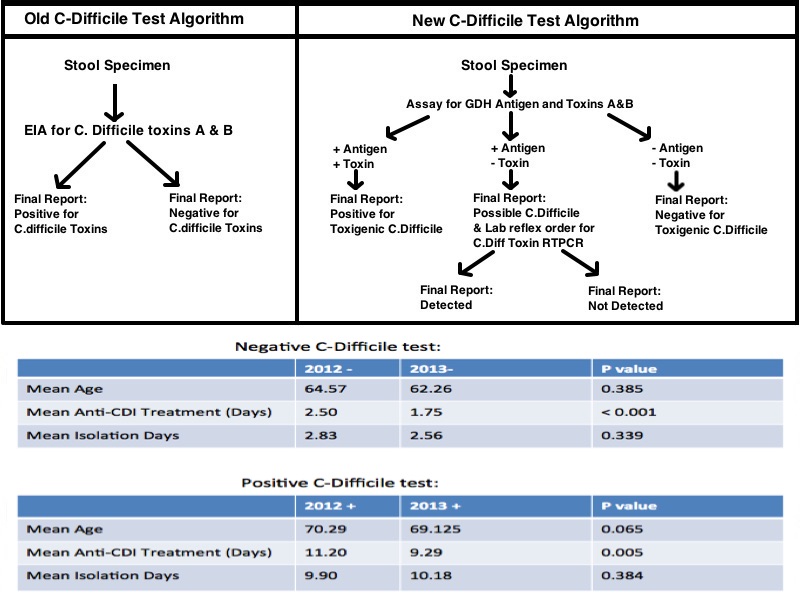
The incidence of Clostridium difficile infection (CDI) and its associated mortality have increased markedly across North America and Europe during the last decade; making CDI one of the most common preventable healthcare-associated conditions. In order to decrease morbidity and mortality and to prevent transmission of CDI within healthcare facilities, clinicians must maintain a high level of suspicion for CDI, and must rapidly institute contact precautions and initiate empiric anti-C. difficile therapy when CDI is suspected. The availability of rapid and reliable diagnosis of CDI potentially enables more appropriate use of antimicrobials and isolation resources. In June 2013, our laboratory converted from an enzyme immunoassay test for C. difficile Toxins A & B to a 2-step testing algorithm (figure 1). The aim of this retrospective study is to compare the management of suspected CDI prior to and following the transition to the 2-step testing algorithm, with specific attention to duration of anti- C. difficile therapy and utilization of isolation resources.
Methods:
This IRB approved study is a retrospective chart review of patients hospitalized at Mount Sinai St. Luke’s and Mount Sinai West Hospitals who were tested for CDI respectively with the old algorithm from October 2012 to December 2012 (Group 1) and the new 2-step algorithm from October 2013 to December 2013 (Group 2). Using the hospitals electronic medical record (EMR), demographic characteristics (age, gender), duration of contact precautions, duration of antimicrobial treatment and C. difficile test results were collected. Characteristics for the CDI-Positive and CDI-Negative patients from Group 1 were compared with those for CDI-Positive and CDI- Negative patients in Group 2. Statistical analysis using Chi Square was performed. A p value below 0.05 was considered statistically significant.
Results:
The age distribution of patients in Group 1 (N=268, 53% female, 47% male, mean age of 65.5 years did not differ significantly from patients in Group 2 (N=255, 51% female, 49% male, mean age of 63.6 years). The most notable finding was a decreased duration of anti-CDI therapy for patients in Group 2. Of interest, the decreased duration of therapy was statistically significant for CDI-Positive patients, as well as for the CDI-negative patients who had been receiving empiric therapy. In addition, the use of isolation measures represented by contact precautions/isolation days was decreased for the CDI-negative patients in Group 2 by 0.27 days (6.5 hours), but did not reach statistical significance.
Conclusions:
The implementation of a high sensitivity 2-step testing algorithm was associated with an overall decrease in anti-CDI antibiotic use that was statistically significant. Our results suggest that the increased sensitivity and specificity of the 2-step testing protocol allows clinicians to limit unnecessary empiric treatment and thereby reduce the risk of emerging resistance and other adverse effect by minimizing the patient’s exposure. Although the decrease in isolation days for CDI-negative patients did not reach statistical significance numerically during the study period, a decrease of 0.27 days (6.5 hours) may have benefits for availability of isolation beds and patient throughout. Our results indicate that a change in the diagnostic approach for CDI has far reaching implications for the overall care for CDI. It remains to be proven if outcome measures such as length of stay, recurrence, mortality and morbidity will also be affected.