Background:
Delays in the discharge process of hospitalized patients impact patient flow and lead to increased costs and slower progression of care. As hospitalist work becomes increasingly shift based, there are concerns for proper patient handoffs and hesitancy with clinical progression of care overnight. This leads to daytime patient flow congestion and is a significant patient quality and safety issue. The Joint Commission has responded by implementing a leadership standard asking hospitals to manage the flow of patients through the hospital, measure efficiency of patient care areas and use data to drive improvements in patient flow processes. The results of improving flow can include increased access, lower costs, better patient experiences and better outcomes.
Purpose:
We developed a 24 hour care progression bundle implementation to focus upon communication, interdisciplinary teamwork, night staff engagement, clinical progression of care, proactive order clarification and shared discharge planning. We hypothesized that this would lead to timely discharges, improved patient flow, and decreased lengths of stay (LOS) and costs. At the time of patient discharge, families should have completed their education teach back sessions, transportation should have already been arranged and discharge medications prescribed. Our primary outcome was a measurement of the time from placement of the discharge order to the time of patient leaving the room (discharge time). Secondary outcome included overall average length of stay (LOS).
Description:
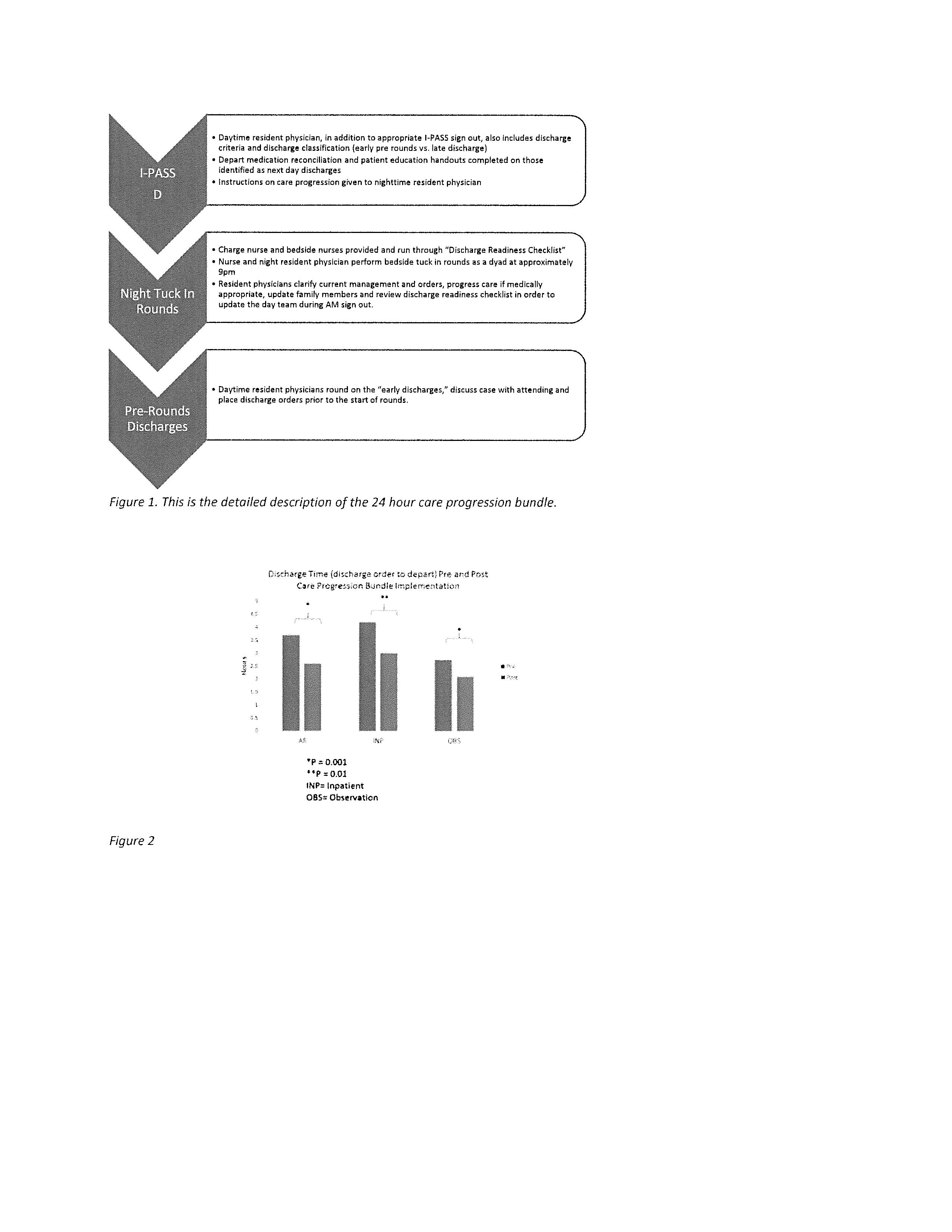
The care progression bundle included: I-PASS Discharge handoffs, night physician and charge nurse bedside “tuck in rounds” and pre-round discharges in the morning (Figure 1). The bundle incorporated a discharge checklist from the physician and nursing standpoint to ensure prescriptions were appropriately sent and filled, transportation arranged and patient education completed prior to placement of the discharge order. At a single tertiary care free-standing children’s hospital, the care progression bundle was piloted in March 2015. We compared average LOS, mean time of discharge and discharge time six months prior (N= 601 patients from Sept 2014- Feb 2015) and six months post implementation (N= 616 patients from April 2015 to Sept 2015) of the care progression bundle.
Conclusions:
Discharge time decreased by 30% from 2.45 hours during the pre-intervention period to 1.76 hours post-intervention (p=0.001) which approximates a savings of 17.5 patient days (Figure 2). There was also a significant decrease in LOS after the care progression bundle with average LOS dropping from 80 hours to 57.3 hours (p=0.003) . The average time of day patients left the hospital was significantly earlier (p<0.001), post implementation. The next step will be to measure physician and nursing satisfaction, analyze patient experience and perform an accurate cost analysis.